Monday Poster Session
Category: Liver
P2496 - Unintended Connection
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- JH
John Herndon, MD
Atrium Health
Charlotte, NC
Presenting Author(s)
Award: Presidential Poster Award
John Herndon, MD1, Mark W. Russo, MD, MPH, FACG2
1Atrium Health, Charlotte, NC; 2Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: We present a case of a common clinical problem encountered by gastroenterologists (melena) with a rare underlying etiology. This case highlights the importance of avoiding anchoring on a negative endoscopic evaluation and considering a more uncommon diagnosis based on the patient's history.
Case Description/Methods: A 73yo man with past medical history of DM and HTN who is status post orthotopic liver transplant for HCV/HCC cirrhosis 4 months prior who presents to the hospital with black tarry stools. Patients post op course has been complicated by anastomotic stricture with cholangitis and bile leak requiring ERCP with biliary stent placement. Patient had recent admission 2 weeks prior where he had evaluation for melena, which included a normal EGD and colonoscopy which showed no active bleeding but old blood in entire colon and terminal ileum. Patient was discharge due to resolution of his melena. On this admission, vitals signs were normal. On physical exam, abdomen was soft, non tender, non distended with well healing surgical incision. Laboratory studies demonstrated hemoglobin 7.5 (previously 9.3) with normal liver function tests. CTA abd/pelvic was negative for active bleed in ED. Decision was made for push enteroscopy with plans to deploy video capsule if negative as previously endoscopic evaluations were concerning for small bowel bleeding. Endoscopic evaluation showed bright red blood refluxing into stomach, copious amount of bright red blood in duodenum with active spurting of blood coming from ampulla. Patient was immediately sent to IR with selective arteriography which showed a focal angulation of the right hepatic artery at the level of the metallic biliary stent which suggest extrinisic compression of the right hepatic artery. Catheter was able to be advanced from right hepatic artery into the common bile duct confirming fistulization. Embolization was not attempted due to concern for liver ischemia and patient was taken emergently to surgery for ligation and resection of the hepatic artery at the level of the fistula. After surgery patient had no further bleeding and continued to have excellent liver function.
Discussion: Arterio-biliary fistulas are a rare cause of upper GI bleeds but should be considered in patients with recent history of biliary tract instrumentation. This case illustrates the importance of a multidisciplinary approach that involved hepatology, gastroenterology, transplant surgery and interventional radiology.

Disclosures:
John Herndon, MD1, Mark W. Russo, MD, MPH, FACG2. P2496 - Unintended Connection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
John Herndon, MD1, Mark W. Russo, MD, MPH, FACG2
1Atrium Health, Charlotte, NC; 2Atrium Health Carolinas Medical Center, Charlotte, NC
Introduction: We present a case of a common clinical problem encountered by gastroenterologists (melena) with a rare underlying etiology. This case highlights the importance of avoiding anchoring on a negative endoscopic evaluation and considering a more uncommon diagnosis based on the patient's history.
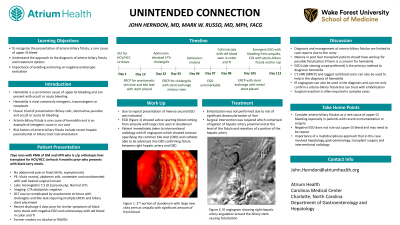
Case Description/Methods: A 73yo man with past medical history of DM and HTN who is status post orthotopic liver transplant for HCV/HCC cirrhosis 4 months prior who presents to the hospital with black tarry stools. Patients post op course has been complicated by anastomotic stricture with cholangitis and bile leak requiring ERCP with biliary stent placement. Patient had recent admission 2 weeks prior where he had evaluation for melena, which included a normal EGD and colonoscopy which showed no active bleeding but old blood in entire colon and terminal ileum. Patient was discharge due to resolution of his melena. On this admission, vitals signs were normal. On physical exam, abdomen was soft, non tender, non distended with well healing surgical incision. Laboratory studies demonstrated hemoglobin 7.5 (previously 9.3) with normal liver function tests. CTA abd/pelvic was negative for active bleed in ED. Decision was made for push enteroscopy with plans to deploy video capsule if negative as previously endoscopic evaluations were concerning for small bowel bleeding. Endoscopic evaluation showed bright red blood refluxing into stomach, copious amount of bright red blood in duodenum with active spurting of blood coming from ampulla. Patient was immediately sent to IR with selective arteriography which showed a focal angulation of the right hepatic artery at the level of the metallic biliary stent which suggest extrinisic compression of the right hepatic artery. Catheter was able to be advanced from right hepatic artery into the common bile duct confirming fistulization. Embolization was not attempted due to concern for liver ischemia and patient was taken emergently to surgery for ligation and resection of the hepatic artery at the level of the fistula. After surgery patient had no further bleeding and continued to have excellent liver function.
Discussion: Arterio-biliary fistulas are a rare cause of upper GI bleeds but should be considered in patients with recent history of biliary tract instrumentation. This case illustrates the importance of a multidisciplinary approach that involved hepatology, gastroenterology, transplant surgery and interventional radiology.

Figure: IR angiogram showing right hepatic artery angulation around the biliary stent causing fistulization.
Disclosures:
John Herndon indicated no relevant financial relationships.
Mark Russo indicated no relevant financial relationships.
John Herndon, MD1, Mark W. Russo, MD, MPH, FACG2. P2496 - Unintended Connection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

