Monday Poster Session
Category: Liver
P2497 - A Case of Delayed Immune Checkpoint Inhibitor Hepatitis in a Patient With Malignant Melanoma
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Dayna M. Telken, DO
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Award: Presidential Poster Award
Dayna M. Telken, DO1, Victor Arce Gutierrez, MD1, Donald Tschirhart, MD2, Yasmin Alishahi, MD3
1University of Arizona College of Medicine, Phoenix, AZ; 2VA Medical Center Phoenix, Phoenix, AZ; 3University of Arizona, Phoenix, AZ
Introduction: Immune checkpoint inhibitors are an increasingly utilized class of medications in oncology. Significant adverse effects have been reported including hepatitis, which mostly occurs early after initiating treatment. We present a case of a 78 year old patient with a past medical history of malignant melanoma who presented with painless jaundice and elevated liver enzymes and found to have biopsy proven hepatitis secondary to immune checkpoint therapy three years after receiving treatment with pembrolizumab.
Case Description/Methods: The patient was a 78-year-old male with past medical history of recurrent sinusoidal mucosal malignant melanoma status post osteomyelitis of nasopharynx on pembrolizumab for three years who presented with new onset painless jaundice starting three days prior to admission. He received pembrolizumab for the past three years of 200 mg IV, with a dose increase to 400 mg IV 12 months prior to presentation. On exam, he was jaundiced with icteric sclera, non-tender abdomen with no asterixis. Laboratory work up revealed alkaline phosphatase at 1780 IU/L, aspartate aminotransferase 2290 IU/L, alanine aminotransferase 1224 IU/L, bilirubin 10.0 mg/dL and direct bilirubin 7.4 mg/dL. Testing for acute hepatitis, CMV, EBV and HIV was negative. Abdominal computed tomography demonstrated marked gallbladder wall thickening and periportal edema and ultrasound doppler of biliary tree demonstrated patent hepatic and portal vessels. Trans jugular biopsy demonstrated expanded portal tracts with evidence of fibrosis and infiltrates composed mostly of lymphocytes with scattered neutrophils histologically suggestive of check point inhibitor hepatitis. The decision was made to start the patient on intravenous methylprednisolone 1 mg/kg/day for three days and sent home on prednisone taper with resolution of liver enzymes after 6 weeks.
Discussion: Immune checkpoint inhibitors are commonly used medications in the field of oncology; however, have been associated with significant gastrointestinal side effects including hepatitis. Most immune related adverse events have been shown to occur 8-12 weeks after starting treatment. Our case involved a patient who presented with asymptomatic jaundice secondary to pembrolizumab therapy, three years after receiving the first dose. Due to the increased frequency of immune checkpoint inhibitors for oncologic treatment, it is important for clinicians to recognize their immune related adverse effects and varying timing in which these toxicities may occur.

Disclosures:
Dayna M. Telken, DO1, Victor Arce Gutierrez, MD1, Donald Tschirhart, MD2, Yasmin Alishahi, MD3. P2497 - A Case of Delayed Immune Checkpoint Inhibitor Hepatitis in a Patient With Malignant Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Dayna M. Telken, DO1, Victor Arce Gutierrez, MD1, Donald Tschirhart, MD2, Yasmin Alishahi, MD3
1University of Arizona College of Medicine, Phoenix, AZ; 2VA Medical Center Phoenix, Phoenix, AZ; 3University of Arizona, Phoenix, AZ
Introduction: Immune checkpoint inhibitors are an increasingly utilized class of medications in oncology. Significant adverse effects have been reported including hepatitis, which mostly occurs early after initiating treatment. We present a case of a 78 year old patient with a past medical history of malignant melanoma who presented with painless jaundice and elevated liver enzymes and found to have biopsy proven hepatitis secondary to immune checkpoint therapy three years after receiving treatment with pembrolizumab.
Case Description/Methods: The patient was a 78-year-old male with past medical history of recurrent sinusoidal mucosal malignant melanoma status post osteomyelitis of nasopharynx on pembrolizumab for three years who presented with new onset painless jaundice starting three days prior to admission. He received pembrolizumab for the past three years of 200 mg IV, with a dose increase to 400 mg IV 12 months prior to presentation. On exam, he was jaundiced with icteric sclera, non-tender abdomen with no asterixis. Laboratory work up revealed alkaline phosphatase at 1780 IU/L, aspartate aminotransferase 2290 IU/L, alanine aminotransferase 1224 IU/L, bilirubin 10.0 mg/dL and direct bilirubin 7.4 mg/dL. Testing for acute hepatitis, CMV, EBV and HIV was negative. Abdominal computed tomography demonstrated marked gallbladder wall thickening and periportal edema and ultrasound doppler of biliary tree demonstrated patent hepatic and portal vessels. Trans jugular biopsy demonstrated expanded portal tracts with evidence of fibrosis and infiltrates composed mostly of lymphocytes with scattered neutrophils histologically suggestive of check point inhibitor hepatitis. The decision was made to start the patient on intravenous methylprednisolone 1 mg/kg/day for three days and sent home on prednisone taper with resolution of liver enzymes after 6 weeks.
Discussion: Immune checkpoint inhibitors are commonly used medications in the field of oncology; however, have been associated with significant gastrointestinal side effects including hepatitis. Most immune related adverse events have been shown to occur 8-12 weeks after starting treatment. Our case involved a patient who presented with asymptomatic jaundice secondary to pembrolizumab therapy, three years after receiving the first dose. Due to the increased frequency of immune checkpoint inhibitors for oncologic treatment, it is important for clinicians to recognize their immune related adverse effects and varying timing in which these toxicities may occur.

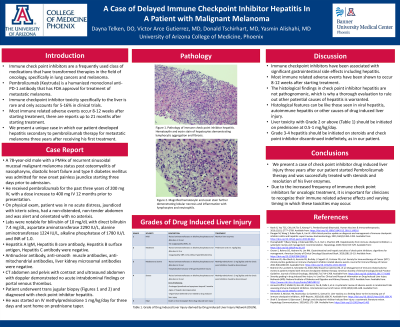
Figure: Pathology of immune check point inhibitor hepatitis. Hematoxylin and eosin stain of hepatocytes demonstrating lymphocytic aggregation and fibrosis.
Disclosures:
Dayna Telken indicated no relevant financial relationships.
Victor Arce Gutierrez indicated no relevant financial relationships.
Donald Tschirhart indicated no relevant financial relationships.
Yasmin Alishahi indicated no relevant financial relationships.
Dayna M. Telken, DO1, Victor Arce Gutierrez, MD1, Donald Tschirhart, MD2, Yasmin Alishahi, MD3. P2497 - A Case of Delayed Immune Checkpoint Inhibitor Hepatitis in a Patient With Malignant Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

