Monday Poster Session
Category: Liver
P2510 - Mogamulizumab-Induced Cholangiopathy in a Patient With Cutaneous T-Cell Lymphoma: A Case Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Hao Chi Zhang, MD
University of Texas MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Rafaela Horrillo, PA-C, Jeannelyn Estrella, MD, Hao Chi Zhang, MD
University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: Mogamulizumab is an antibody that inhibits CC chemokine receptor 4, approved for relapsed mycosis fungoides and Sézary syndrome. While hepatitis B reactivation risk and one case of autoimmune hepatitis had been documented, no specific documentation of mogamulizumab-induced cholangiohepatitis exists. We describe a case in which delayed, new-onset cholangiohepatitis was attributed to long-term use of mogamulizumab maintenance therapy, managed with ursodeoxycholic acid (UDCA), without steroids.
Case Description/Methods: A 78-year-old man with cutaneous T-cell lymphoma on maintenance mogamulizumab since 6/2021 and no prior established history of liver disease was evaluated for elevated liver enzymes. Prior mycosis fungoides treatment included extracorpeal photophoresis (2012-2021), SGN-30 (anti-CD30 mAb) (2012), interferon alfa-2b (2013), and ultraviolet B therapy (2014). He denied use of alcohol and dietary supplements/herbals. Liver enzymes increased to peak ALT 97, AST 82, alkaline phosphatase (ALP) 428, and GGT 472, with a cholestatic pattern of injury, although the bilirubin was normal. Other laboratory studies showed: elevated total IgG (1,711) and IgM (247), antinuclear antibody positive (1:640). Abdominal MRI/MRCP did not show intra- or extrahepatic biliary abnormalities. Parenchymal liver biopsy revealed biliary pattern of injury characterized by mixed portal inflammation with epithelioid non-necrotizing granulomas, cholangitis with bile duct epithelial injury, bile ductular proliferation, and portal and periportal fibrosis. The portal inflammation was composed of lymphocytes, plasma cells, eosinophils and neutrophils. The findings were not compatible with autoimmune hepatitis or primary biliary cholangitis. Due to cholangiopathic features with high ALP and GGT, UDCA (13.8 mg/kg) was initiated. ALP and GGT improved, with complete normalization of ALT and AST even after the patient resumed treatment with mogamulizumab.
Discussion: Detailed reports are scarce regarding the nature of and treatment of mogamulizumab-induced liver injury. The documented cases highlight transient liver injury that spontaneously resolves. Our case also highlights the role of UDCA to treat this drug-induced cholangiohepatitis, without need for steroids, and even permitting the patient to continue the same culprit drug as maintenance without recurrent liver injury. The liver biopsy was important for diagnosis. More data are needed to characterize the spectrum of and behavior of mogamulizumab-induced liver injury.

Disclosures:
Rafaela Horrillo, PA-C, Jeannelyn Estrella, MD, Hao Chi Zhang, MD. P2510 - Mogamulizumab-Induced Cholangiopathy in a Patient With Cutaneous T-Cell Lymphoma: A Case Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: Mogamulizumab is an antibody that inhibits CC chemokine receptor 4, approved for relapsed mycosis fungoides and Sézary syndrome. While hepatitis B reactivation risk and one case of autoimmune hepatitis had been documented, no specific documentation of mogamulizumab-induced cholangiohepatitis exists. We describe a case in which delayed, new-onset cholangiohepatitis was attributed to long-term use of mogamulizumab maintenance therapy, managed with ursodeoxycholic acid (UDCA), without steroids.
Case Description/Methods: A 78-year-old man with cutaneous T-cell lymphoma on maintenance mogamulizumab since 6/2021 and no prior established history of liver disease was evaluated for elevated liver enzymes. Prior mycosis fungoides treatment included extracorpeal photophoresis (2012-2021), SGN-30 (anti-CD30 mAb) (2012), interferon alfa-2b (2013), and ultraviolet B therapy (2014). He denied use of alcohol and dietary supplements/herbals. Liver enzymes increased to peak ALT 97, AST 82, alkaline phosphatase (ALP) 428, and GGT 472, with a cholestatic pattern of injury, although the bilirubin was normal. Other laboratory studies showed: elevated total IgG (1,711) and IgM (247), antinuclear antibody positive (1:640). Abdominal MRI/MRCP did not show intra- or extrahepatic biliary abnormalities. Parenchymal liver biopsy revealed biliary pattern of injury characterized by mixed portal inflammation with epithelioid non-necrotizing granulomas, cholangitis with bile duct epithelial injury, bile ductular proliferation, and portal and periportal fibrosis. The portal inflammation was composed of lymphocytes, plasma cells, eosinophils and neutrophils. The findings were not compatible with autoimmune hepatitis or primary biliary cholangitis. Due to cholangiopathic features with high ALP and GGT, UDCA (13.8 mg/kg) was initiated. ALP and GGT improved, with complete normalization of ALT and AST even after the patient resumed treatment with mogamulizumab.
Discussion: Detailed reports are scarce regarding the nature of and treatment of mogamulizumab-induced liver injury. The documented cases highlight transient liver injury that spontaneously resolves. Our case also highlights the role of UDCA to treat this drug-induced cholangiohepatitis, without need for steroids, and even permitting the patient to continue the same culprit drug as maintenance without recurrent liver injury. The liver biopsy was important for diagnosis. More data are needed to characterize the spectrum of and behavior of mogamulizumab-induced liver injury.

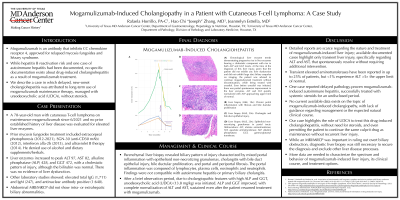
Figure: (A) Chronological liver enzyme trends demonstrating progressive rise in liver enzymes bearing a cholestatic component with rise in both ALP and GGT levels. At the time of the diagnosis of this liver injury, given that the patient did not exhibit any liver dysfunction and did not exhibit large duct biliary sequelae on imaging, the patient was advised to continue mogamulizumab treatment without discontinuation, while being treated with ursodiol. Even before ursodiol was initiated, there was partial spontaneous improvement in the liver enzymes. ALT and AST quickly normalized with ALP approaching upper limit of normal. (B) Liver biopsy (H&E, 10x): Chronic portal inflammation with fibrosis and bile ductular proliferation. (C) Liver biopsy (H&E, 20x): Cholangitis and bile duct epithelial injury. (D) Liver biopsy (H&E, 20x): Epithelioid non-necrotizing granulomas in portal tracts.
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; GGT, gamma-glutamyl transferase.
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALP, alkaline phosphatase; GGT, gamma-glutamyl transferase.
Disclosures:
Rafaela Horrillo indicated no relevant financial relationships.
Jeannelyn Estrella indicated no relevant financial relationships.
Hao Chi Zhang indicated no relevant financial relationships.
Rafaela Horrillo, PA-C, Jeannelyn Estrella, MD, Hao Chi Zhang, MD. P2510 - Mogamulizumab-Induced Cholangiopathy in a Patient With Cutaneous T-Cell Lymphoma: A Case Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
