Monday Poster Session
Category: Liver
P2511 - Colon Cleanse Revenge Fenbendazole Causes Severe Drug-Induced Liver Injury
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

John Green, DO, MPH
University of South Alabama
Mobile, AL
Presenting Author(s)
Alvin Green, DO, MPH, Phillip Henderson, DO
University of South Alabama, Mobile, AL
Introduction: Drug induced liver injury is a worldwide disease with an estimated incidence of 14-24 case per 100,000 people. Antibiotics and herbal or dietary supplements are the most common cause of DILI. In the internet age people have access to information and medications not previously available which allow patients access to substances that may be harmful to their health.
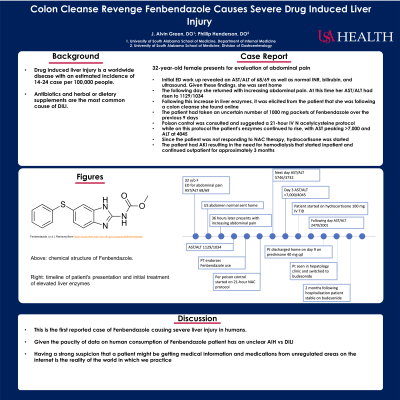
Case Description/Methods: We present a 32-year-old female with no pmh who presented with a chief complaint of abdominal pain nausea and vomiting for the past 3 days. Initial ED work up revealed an AST/ALT of 68/69 as well as normal INR, bilirubin and ultrasound. Given these findings she was sent home. The following day she returned with increasing abdominal pain. At this time her AST/ALT had risen to 1129/1034. Following this increase in liver enzymes, it was elicited from the patient that she was following a colon cleanse she found online. It consisted centered around Fenbendazole as the bowel cleanse agent. The patient had taken an uncertain number of 1000 mg packets of Fenbendazole over the previous 9 days. Poison control was consulted and suggested a 21-hour IV N acetylcysteine protocol. However, while on this protocol the patient’s enzymes continued to rise, with both ALT and AST peaking at >7,000. Thus, the patient was determined not responding to NAC therapy and Cortef was started. The following morning her labs had dropped to an AST/ALT of 2,389 and 3,132. During this whole process the patient’s INR reached a max of 2.8 and her bilirubin never rose above 1.7. In addition, she never had any change in mental status. Therefore, while there were concerns for acute liver failure requiring a transplant, she never required transfer to a transplant center. After 9 days of hospitalization the patient’s labs had stabilized and she was transitioned to oral prednisone and discharged to follow up in hepatology clinic. Her work up for hereditary, autoimmune hepatitis and viral hepatitis all came back negative. Patient has had no return of symptoms with normal biochemical markers and continues low dose Budesonide.
Discussion: This is the first reported case of Fenbendazole causing severe liver injury in humans. Given the increasing extension of the internet into every aspect of life it is unsurprising that medical field is influenced by its spread. Having a strong suspicion that a patient might be getting medical information and medications from unregulated areas on the internet is the reality of the world in which we practice.

Disclosures:
Alvin Green, DO, MPH, Phillip Henderson, DO. P2511 - Colon Cleanse Revenge Fenbendazole Causes Severe Drug-Induced Liver Injury, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of South Alabama, Mobile, AL
Introduction: Drug induced liver injury is a worldwide disease with an estimated incidence of 14-24 case per 100,000 people. Antibiotics and herbal or dietary supplements are the most common cause of DILI. In the internet age people have access to information and medications not previously available which allow patients access to substances that may be harmful to their health.
Case Description/Methods: We present a 32-year-old female with no pmh who presented with a chief complaint of abdominal pain nausea and vomiting for the past 3 days. Initial ED work up revealed an AST/ALT of 68/69 as well as normal INR, bilirubin and ultrasound. Given these findings she was sent home. The following day she returned with increasing abdominal pain. At this time her AST/ALT had risen to 1129/1034. Following this increase in liver enzymes, it was elicited from the patient that she was following a colon cleanse she found online. It consisted centered around Fenbendazole as the bowel cleanse agent. The patient had taken an uncertain number of 1000 mg packets of Fenbendazole over the previous 9 days. Poison control was consulted and suggested a 21-hour IV N acetylcysteine protocol. However, while on this protocol the patient’s enzymes continued to rise, with both ALT and AST peaking at >7,000. Thus, the patient was determined not responding to NAC therapy and Cortef was started. The following morning her labs had dropped to an AST/ALT of 2,389 and 3,132. During this whole process the patient’s INR reached a max of 2.8 and her bilirubin never rose above 1.7. In addition, she never had any change in mental status. Therefore, while there were concerns for acute liver failure requiring a transplant, she never required transfer to a transplant center. After 9 days of hospitalization the patient’s labs had stabilized and she was transitioned to oral prednisone and discharged to follow up in hepatology clinic. Her work up for hereditary, autoimmune hepatitis and viral hepatitis all came back negative. Patient has had no return of symptoms with normal biochemical markers and continues low dose Budesonide.
Discussion: This is the first reported case of Fenbendazole causing severe liver injury in humans. Given the increasing extension of the internet into every aspect of life it is unsurprising that medical field is influenced by its spread. Having a strong suspicion that a patient might be getting medical information and medications from unregulated areas on the internet is the reality of the world in which we practice.

Figure: Chemical formula of febendazole
Disclosures:
Alvin Green indicated no relevant financial relationships.
Phillip Henderson indicated no relevant financial relationships.
Alvin Green, DO, MPH, Phillip Henderson, DO. P2511 - Colon Cleanse Revenge Fenbendazole Causes Severe Drug-Induced Liver Injury, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
