Monday Poster Session
Category: Liver
P2514 - Epstein-Barr Virus Related Acute Liver Failure in a Young Immunocompetent Male
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Fredella Lee, MD
New York Presbyterian Weill Cornell Medical Center
Westwood, MA
Presenting Author(s)
Fredella Lee, MD1, He Qiu, MD2, Ali Wakil, MD2, Raquel Olivo-Salcedo, MD, MPH2
1New York Presbyterian Weill Cornell Medical Center, New York, NY; 2Rutgers New Jersey Medical School, Newark, NJ
Introduction: Epstein-Barr virus (EBV) is commonly associated with infectious mononucleosis, although acute liver failure (ALF) secondary to primary EBV infection is rare. Patients are often asymptomatic or can present with fever, pharyngitis, lymphadenopathy, malaise, and less commonly hepatitis or splenomegaly. We present a case of EBV-associated ALF in an immunocompetent patient who underwent an orthotopic liver transplant (OLT).
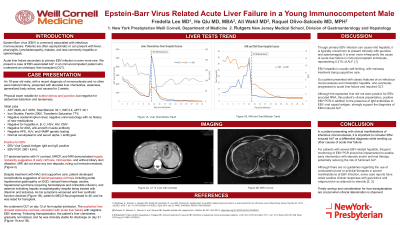
Case Description/Methods: An 18-year-old Hispanic male, who had a recent history of mononucleosis, presented with elevated liver chemistries, weakness, body aches, and nausea for 2 weeks. His blood work on presentation showed AST 2649, ALT 2876, Tbili 33.1, INR 2.4, and aPTT 39.1. His ferritin and transferrin saturation were elevated at 2000 and 77% respectively, but hemochromatosis genetic test was negative. Urinary toxicology screen was unremarkable. Extensive diagnostic workup ruled out other causes of acute liver injury, including negative cytomegalovirus, HSV, alpha-1 antitrypsin deficiency, Wilson’s disease, autoimmune hepatitis, acute hepatitis A and B, and hepatitis C ab. He tested positive for EBV IgM and IgG, with EBV PCR of 2601 IU/mL, confirming acute EBV infection. Imaging studies demonstrated cirrhosis, mild ascites but no biliary duct dilation. Despite receiving N-acetylcysteine and aggressive supportive care, the patient developed worsening encephalopathy necessitating hemodialysis and listing for liver transplant with MELD-Na of 46. On day 12, the patient underwent OLT. The explanted liver showed extensive necrosis consistent with acute liver failure with negative EBV staining. Following transplantation, the patient’s liver chemistries gradually normalized, and he was clinically stable for discharge on day 31.
Discussion: This case highlights the importance of considering EBV-induced ALF in patients presenting with clinical manifestations of mononucleosis and ruling out other causes of acute liver failure. Despite the absence of EBV staining in the explanted liver, this patient's clinical presentation and positive EBV PCR strongly support the diagnosis of EBV-induced ALF. For patients with severe EBV-related hepatitis, frequent monitoring of EBV PCR should be implemented to enable early intervention with steroids and/or antiviral therapy, potentially reducing the risk of fulminant ALF. Timely workup and consideration for liver transplantation are crucial when clinical deterioration is observed.

Disclosures:
Fredella Lee, MD1, He Qiu, MD2, Ali Wakil, MD2, Raquel Olivo-Salcedo, MD, MPH2. P2514 - Epstein-Barr Virus Related Acute Liver Failure in a Young Immunocompetent Male, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1New York Presbyterian Weill Cornell Medical Center, New York, NY; 2Rutgers New Jersey Medical School, Newark, NJ
Introduction: Epstein-Barr virus (EBV) is commonly associated with infectious mononucleosis, although acute liver failure (ALF) secondary to primary EBV infection is rare. Patients are often asymptomatic or can present with fever, pharyngitis, lymphadenopathy, malaise, and less commonly hepatitis or splenomegaly. We present a case of EBV-associated ALF in an immunocompetent patient who underwent an orthotopic liver transplant (OLT).
Case Description/Methods: An 18-year-old Hispanic male, who had a recent history of mononucleosis, presented with elevated liver chemistries, weakness, body aches, and nausea for 2 weeks. His blood work on presentation showed AST 2649, ALT 2876, Tbili 33.1, INR 2.4, and aPTT 39.1. His ferritin and transferrin saturation were elevated at 2000 and 77% respectively, but hemochromatosis genetic test was negative. Urinary toxicology screen was unremarkable. Extensive diagnostic workup ruled out other causes of acute liver injury, including negative cytomegalovirus, HSV, alpha-1 antitrypsin deficiency, Wilson’s disease, autoimmune hepatitis, acute hepatitis A and B, and hepatitis C ab. He tested positive for EBV IgM and IgG, with EBV PCR of 2601 IU/mL, confirming acute EBV infection. Imaging studies demonstrated cirrhosis, mild ascites but no biliary duct dilation. Despite receiving N-acetylcysteine and aggressive supportive care, the patient developed worsening encephalopathy necessitating hemodialysis and listing for liver transplant with MELD-Na of 46. On day 12, the patient underwent OLT. The explanted liver showed extensive necrosis consistent with acute liver failure with negative EBV staining. Following transplantation, the patient’s liver chemistries gradually normalized, and he was clinically stable for discharge on day 31.
Discussion: This case highlights the importance of considering EBV-induced ALF in patients presenting with clinical manifestations of mononucleosis and ruling out other causes of acute liver failure. Despite the absence of EBV staining in the explanted liver, this patient's clinical presentation and positive EBV PCR strongly support the diagnosis of EBV-induced ALF. For patients with severe EBV-related hepatitis, frequent monitoring of EBV PCR should be implemented to enable early intervention with steroids and/or antiviral therapy, potentially reducing the risk of fulminant ALF. Timely workup and consideration for liver transplantation are crucial when clinical deterioration is observed.

Figure: Figure A demonstrates change in patient's liver chemistries over his hospital course. Figure B demonstrates change in patient's INR and total bilirubin over his hospital course.
Disclosures:
Fredella Lee indicated no relevant financial relationships.
He Qiu indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Raquel Olivo-Salcedo indicated no relevant financial relationships.
Fredella Lee, MD1, He Qiu, MD2, Ali Wakil, MD2, Raquel Olivo-Salcedo, MD, MPH2. P2514 - Epstein-Barr Virus Related Acute Liver Failure in a Young Immunocompetent Male, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
