Monday Poster Session
Category: Liver
P2516 - A Novel Case of Non-Cirrhotic Portal Hypertension After Hepatic Lobectomy
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Ahmet Sakiri, MD
MercyHealth
Rockford, IL
Presenting Author(s)
Ahmet Sakiri, MD, Mudassar Sandozi, DO, Arshan Chaudhri, MD, Sabah Mahmood, MD, Ghanshyam Patel, MD, Mackenley Pierre, , Yusrah Ahmed, , Usama Altayeh, , Thayer Hamoudah, MD, Altaf Dawood, MD, MBBS, Naser Khan, MD
MercyHealth, Rockford, IL
Introduction: Non-cirrhotic portal hypertension (NCPH) encompasses a group of liver disorders that are classified anatomically by their impact on the hepatic vasculature (pre-hepatic, hepatic, and post-hepatic). We present a unique case of non-cirrhotic portal hypertension secondary to right hepatic lobectomy in a patient with a suspicious appearing hemangioma.
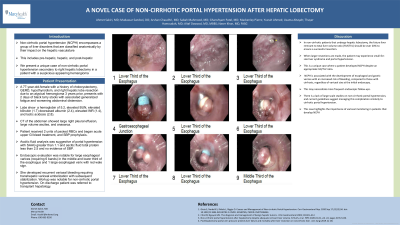
Case Description/Methods: A 77-year-old-female with a history of cholecystectomy, GERD, hypothyroidism, and right hepatic lobe resection due to an atypical hemangioma 3 years prior, presented with 2 days of black tarry stools with associated generalized fatigue and worsening abdominal distension. Notable labs on presentation showed a hemoglobin of 5.2, elevated BUN, elevated bilirubin (1.7) decreased albumin (2.4), elevated INR (1.4), and lactic acidosis (2.8). CT of the abdomen showed large right pleural effusion, large volume ascites, and anasarca. Patient received 2 units of packed RBCs and began acute upper GI bleed treatment, and SBP prophylaxis. Ascitic fluid analysis was suggestive of portal hypertension with SAAG greater than 1.1 and ascitic fluid total protein less than 2.5 and no evidence of SBP. Endoscopic evaluation was notable for large esophageal varices (requiring 6 bands) in the middle and lower third of the esophagus and 1 large esophageal varix with red wale sign. She developed recurrent variceal bleeding requiring transhepatic variceal embolization with subsequent stabilization. Workup was notable for non-cirrhotic portal hypertension. On discharge patient was referred to transplant hepatology.
Discussion: In non-cirrhotic patients that undergo hepatic lobectomy, the future liver remnant to total liver volume ratio (FLR/TLV) should be over 20% to ensure a successful resection. When larger resections are made, the patient may experience small-for-size liver syndrome and portal hypertension. This is a unique case where a patient developed NCPH despite an appropriate FLR/TLV ratio. NCPH is associated with the development of esophageal and gastric varices at an increased risk of bleeding, compared to those with cirrhosis, regardless of variceal size at the initial endoscopy. This may necessitate more frequent endoscopic follow-ups. However, there is a lack of large-scale studies on non-cirrhotic portal hypertension, and current guidelines suggest managing this complication similarly to cirrhotic portal hypertension. This case highlights the importance of variceal monitoring in patients that develop NCPH.

Disclosures:
Ahmet Sakiri, MD, Mudassar Sandozi, DO, Arshan Chaudhri, MD, Sabah Mahmood, MD, Ghanshyam Patel, MD, Mackenley Pierre, , Yusrah Ahmed, , Usama Altayeh, , Thayer Hamoudah, MD, Altaf Dawood, MD, MBBS, Naser Khan, MD. P2516 - A Novel Case of Non-Cirrhotic Portal Hypertension After Hepatic Lobectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
MercyHealth, Rockford, IL
Introduction: Non-cirrhotic portal hypertension (NCPH) encompasses a group of liver disorders that are classified anatomically by their impact on the hepatic vasculature (pre-hepatic, hepatic, and post-hepatic). We present a unique case of non-cirrhotic portal hypertension secondary to right hepatic lobectomy in a patient with a suspicious appearing hemangioma.
Case Description/Methods: A 77-year-old-female with a history of cholecystectomy, GERD, hypothyroidism, and right hepatic lobe resection due to an atypical hemangioma 3 years prior, presented with 2 days of black tarry stools with associated generalized fatigue and worsening abdominal distension. Notable labs on presentation showed a hemoglobin of 5.2, elevated BUN, elevated bilirubin (1.7) decreased albumin (2.4), elevated INR (1.4), and lactic acidosis (2.8). CT of the abdomen showed large right pleural effusion, large volume ascites, and anasarca. Patient received 2 units of packed RBCs and began acute upper GI bleed treatment, and SBP prophylaxis. Ascitic fluid analysis was suggestive of portal hypertension with SAAG greater than 1.1 and ascitic fluid total protein less than 2.5 and no evidence of SBP. Endoscopic evaluation was notable for large esophageal varices (requiring 6 bands) in the middle and lower third of the esophagus and 1 large esophageal varix with red wale sign. She developed recurrent variceal bleeding requiring transhepatic variceal embolization with subsequent stabilization. Workup was notable for non-cirrhotic portal hypertension. On discharge patient was referred to transplant hepatology.
Discussion: In non-cirrhotic patients that undergo hepatic lobectomy, the future liver remnant to total liver volume ratio (FLR/TLV) should be over 20% to ensure a successful resection. When larger resections are made, the patient may experience small-for-size liver syndrome and portal hypertension. This is a unique case where a patient developed NCPH despite an appropriate FLR/TLV ratio. NCPH is associated with the development of esophageal and gastric varices at an increased risk of bleeding, compared to those with cirrhosis, regardless of variceal size at the initial endoscopy. This may necessitate more frequent endoscopic follow-ups. However, there is a lack of large-scale studies on non-cirrhotic portal hypertension, and current guidelines suggest managing this complication similarly to cirrhotic portal hypertension. This case highlights the importance of variceal monitoring in patients that develop NCPH.

Figure: Endoscopic view of esophageal varices and red wale sign (image 2 and 3)
Disclosures:
Ahmet Sakiri indicated no relevant financial relationships.
Mudassar Sandozi indicated no relevant financial relationships.
Arshan Chaudhri indicated no relevant financial relationships.
Sabah Mahmood indicated no relevant financial relationships.
Ghanshyam Patel indicated no relevant financial relationships.
Mackenley Pierre indicated no relevant financial relationships.
Yusrah Ahmed indicated no relevant financial relationships.
Usama Altayeh indicated no relevant financial relationships.
Thayer Hamoudah indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Ahmet Sakiri, MD, Mudassar Sandozi, DO, Arshan Chaudhri, MD, Sabah Mahmood, MD, Ghanshyam Patel, MD, Mackenley Pierre, , Yusrah Ahmed, , Usama Altayeh, , Thayer Hamoudah, MD, Altaf Dawood, MD, MBBS, Naser Khan, MD. P2516 - A Novel Case of Non-Cirrhotic Portal Hypertension After Hepatic Lobectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
