Monday Poster Session
Category: Liver
P2518 - Liver Transplantation in a Stage IV Malignancy: A New Norm
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Sophia Dar, MD
Northshore-Long Island Jewish Medical Center
Springfield , IL
Presenting Author(s)
Rehmat Ullah Awan, MD1, Ambreen Nabeel, MBBS1, Sophia Haroon Dar, MD2, Shazia Rashid, MD3, Ayokunle T.. Abegunde, MD4, Hrishikesh Samant, MD5
1Ochsner Rush Medical Center, Meridian, MS; 2Northshore-Long Island Jewish Medical Center, New York, NY; 3LSU Health Sciences Center, Shreveport, LA; 4Loyola University Medical Center, Maywood, IL; 5Ochsner Medical Center, New Orleans, LA
Introduction: Solid organ transplantation in a stage IV malignancy is relatively unheard of. However, when the course of neoplasm is indolent then exceptions can be made. We describe a case of a rare hepatic malignancy with an even rarer mutation.
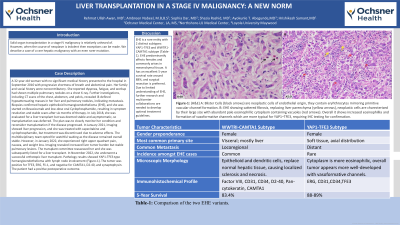
Case Description/Methods: A 32-year-old woman with no significant medical history presented to the hospital in September 2016 with progressive shortness of breath and abdominal pain. Her family and social history were noncontributory. She reported dyspnea, fatigue, and workup had shown multiple pulmonary nodules on a chest X-ray. Further investigations, including CT scans of the chest, abdomen, and pelvis, revealed ill-defined hypoattenuating masses in her liver and pulmonary nodules, indicating metastasis. Biopsies confirmed hepatic epithelioid hemangioendothelioma (EHE), and she was started on Bevacizumab and low-dose oral Cyclophosphamide, resulting in symptom resolution and stable scans after six months of therapy. In July 2018, she was evaluated for a liver transplant but was deemed stable and asymptomatic, so transplantation was deferred. The plan was to closely monitor her condition and reconsider transplantation if the disease progressed. In January 2021, imaging showed liver progression, and she was treated with capecitabine and cyclophosphamide, but treatment was discontinued due to adverse effects. The multidisciplinary team opted for watchful waiting as the disease remained overall stable. However, in January 2022, she experienced right upper quadrant pain, nausea, and weight loss. Imaging revealed increased liver tumor burden but stable pulmonary lesions. The transplant committee reassessed her and she was subsequently listed for a liver transplant. In November 2022, she underwent a successful orthotopic liver transplant. Pathology results showed YAP1-TFE3 type hemangioendothelioma with lymph node involvement (Figure-1). The tumor was positive for TFE3, ERG, Fli-1, and negative for CAMTA1, D2-40, and synaptophysin. The patient had a positive postoperative outcome.
Discussion: EHE is a rare entity with 2 distinct subtypes: YAP1-TFE3 and WWTR1-CAMTA1 subtype (Table-1). EHE predominantly affects females and commonly arises in mesenchymal tissue. It has an excellent 5-year survival rate around 88%, and surgical resection is preferred. Due to limited understanding of EHE, further research and multicenter collaborations are needed to develop optimal treatment guidelines.

Disclosures:
Rehmat Ullah Awan, MD1, Ambreen Nabeel, MBBS1, Sophia Haroon Dar, MD2, Shazia Rashid, MD3, Ayokunle T.. Abegunde, MD4, Hrishikesh Samant, MD5. P2518 - Liver Transplantation in a Stage IV Malignancy: A New Norm, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Ochsner Rush Medical Center, Meridian, MS; 2Northshore-Long Island Jewish Medical Center, New York, NY; 3LSU Health Sciences Center, Shreveport, LA; 4Loyola University Medical Center, Maywood, IL; 5Ochsner Medical Center, New Orleans, LA
Introduction: Solid organ transplantation in a stage IV malignancy is relatively unheard of. However, when the course of neoplasm is indolent then exceptions can be made. We describe a case of a rare hepatic malignancy with an even rarer mutation.
Case Description/Methods: A 32-year-old woman with no significant medical history presented to the hospital in September 2016 with progressive shortness of breath and abdominal pain. Her family and social history were noncontributory. She reported dyspnea, fatigue, and workup had shown multiple pulmonary nodules on a chest X-ray. Further investigations, including CT scans of the chest, abdomen, and pelvis, revealed ill-defined hypoattenuating masses in her liver and pulmonary nodules, indicating metastasis. Biopsies confirmed hepatic epithelioid hemangioendothelioma (EHE), and she was started on Bevacizumab and low-dose oral Cyclophosphamide, resulting in symptom resolution and stable scans after six months of therapy. In July 2018, she was evaluated for a liver transplant but was deemed stable and asymptomatic, so transplantation was deferred. The plan was to closely monitor her condition and reconsider transplantation if the disease progressed. In January 2021, imaging showed liver progression, and she was treated with capecitabine and cyclophosphamide, but treatment was discontinued due to adverse effects. The multidisciplinary team opted for watchful waiting as the disease remained overall stable. However, in January 2022, she experienced right upper quadrant pain, nausea, and weight loss. Imaging revealed increased liver tumor burden but stable pulmonary lesions. The transplant committee reassessed her and she was subsequently listed for a liver transplant. In November 2022, she underwent a successful orthotopic liver transplant. Pathology results showed YAP1-TFE3 type hemangioendothelioma with lymph node involvement (Figure-1). The tumor was positive for TFE3, ERG, Fli-1, and negative for CAMTA1, D2-40, and synaptophysin. The patient had a positive postoperative outcome.
Discussion: EHE is a rare entity with 2 distinct subtypes: YAP1-TFE3 and WWTR1-CAMTA1 subtype (Table-1). EHE predominantly affects females and commonly arises in mesenchymal tissue. It has an excellent 5-year survival rate around 88%, and surgical resection is preferred. Due to limited understanding of EHE, further research and multicenter collaborations are needed to develop optimal treatment guidelines.

Figure: Figure-1: (H&E) A: Blister Cells (black arrows) are neoplastic cells of endothelial origin, they contain eryhthrocytes mirroring primitive vascular channel formation. B: EHE showing sattered fibrosis, replacing liver parenchyma (yellow arrows), neoplastic cells are charecterised by their large size with abundant pale eosinophillic cytoplasm containing vacuoles (red arrows). Overall it shows increased eosinophillia and formation of vasoformative channels which are more typical for YAP1–TFE3, requiring IHC testing for confirmation.
Disclosures:
Rehmat Ullah Awan indicated no relevant financial relationships.
Ambreen Nabeel indicated no relevant financial relationships.
Sophia Haroon Dar indicated no relevant financial relationships.
Shazia Rashid indicated no relevant financial relationships.
Ayokunle Abegunde indicated no relevant financial relationships.
Hrishikesh Samant indicated no relevant financial relationships.
Rehmat Ullah Awan, MD1, Ambreen Nabeel, MBBS1, Sophia Haroon Dar, MD2, Shazia Rashid, MD3, Ayokunle T.. Abegunde, MD4, Hrishikesh Samant, MD5. P2518 - Liver Transplantation in a Stage IV Malignancy: A New Norm, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
