Monday Poster Session
Category: Liver
P2519 - Rapidly Progressive Primary Biliary Cholangitis and Autoimmune Hepatitis Associated with Turmeric-Containing Supplements
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Iqra Kazi, MD
UT Health San Antonio
San Antonio, TX
Presenting Author(s)
Iqra Kazi, MD1, Lisa Pedicone, PhD2, Jan Petrasek, MD, PhD3, Carmen Landaverde, MD4, Fabian Rodas, MD4, Eugenia Tsai, MD4, Eric Lawitz, MD4, Fred Poordad, MD4
1UT Health San Antonio, San Antonio, TX; 2Texas Liver Institute, San Antonio, TX; 3UT Health San Antonio, Texas Liver Institute, Jackson, MS; 4UT Health San Antonio, Texas Liver Institute, San Antonio, TX
Introduction: Herbal supplement use has increased worldwide. We present a patient who used supplements with high doses of turmeric associated with primary biliary cholangitis (PBC).
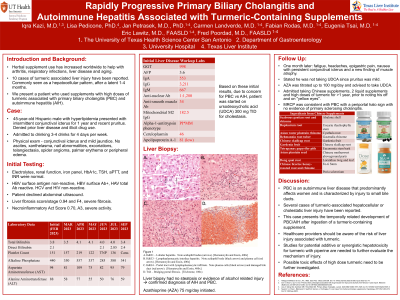
Case Description/Methods: A 45-year-old Hispanic male with hyperlipidemia presented with intermittent conjunctival icterus for one year and recent pruritus. He denied prior liver disease and illicit drug use but admitted to drinking 3-4 drinks x 4 days/wk. Physical exam: Conjunctival icterus and mild jaundice. No ascites, xanthelasma, nail abnormalities, excoriations, telangiectasia, spider angioma, palmar erythema or peripheral edema noted. Initial labs shown in Table 1. Electrolytes, renal function, iron panel, HbA1c, TSH, aPTT, and INR were normal. HBV sAg-, HBV surface Ab+, HCV and HIV non-reactive. Patient declined abdominal ultrasound. Other labs revealed GGT 998, AFP 3.6, ANA 1:1280, IgA 553, IgG 3211, IgM 667, mitochondrial Ab 182.5, alpha-1-antitrypsin phenotype PI*MM, ceruloplasmin 46. Differential diagnosis included PBC vs autoimmune hepatitis (AIH). He was started on ursodeoxycholic acid (UDCA) 300 mg TID for cholestasis.
Liver biopsy revealed chronic lymphoplasmacytic portal hepatitis with ductopenia and bridging fibrosis, stage 3/4. Focal interface hepatitis with plasma cell clusters was present. The lobular parenchyma showed scattered lymphohistiocytic and plasma cell infiltrates along with pseudoduct formation and focal intracellular cholestasis. No steatosis or evidence of alcohol related injury. This confirmed the diagnosis of AIH and PBC. Azathioprine (AZA) 75 mg/day was started for presumed AIH.
One month later, he had fatigue, headaches, epigastric pain, and nausea with persistent conjunctival icterus and a new finding of muscle atrophy. He revealed he had not taken UDCA since pruritus was mild. AZA was titrated up to 100 mg/day and he was advised to take UDCA. The patient admitted taking high doses of turmeric for >1 year, prior to noting his off and on "yellow eyes". MRCP was consistent with PBC with a periportal halo sign with no evidence of primary sclerosing cholangitis.
Discussion: PBC is an autoimmune liver disease that predominantly affects women and is characterized by injury to small bile ducts. Several cases of turmeric-associated hepatocellular or cholestatic liver injury have been reported. This case presents the temporally related development of PBC/AIH after ingestion of a turmeric-containing supplement. Possible toxic effects of high dose turmeric need to be further investigated.
Disclosures:
Iqra Kazi, MD1, Lisa Pedicone, PhD2, Jan Petrasek, MD, PhD3, Carmen Landaverde, MD4, Fabian Rodas, MD4, Eugenia Tsai, MD4, Eric Lawitz, MD4, Fred Poordad, MD4. P2519 - Rapidly Progressive Primary Biliary Cholangitis and Autoimmune Hepatitis Associated with Turmeric-Containing Supplements, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UT Health San Antonio, San Antonio, TX; 2Texas Liver Institute, San Antonio, TX; 3UT Health San Antonio, Texas Liver Institute, Jackson, MS; 4UT Health San Antonio, Texas Liver Institute, San Antonio, TX
Introduction: Herbal supplement use has increased worldwide. We present a patient who used supplements with high doses of turmeric associated with primary biliary cholangitis (PBC).
Case Description/Methods: A 45-year-old Hispanic male with hyperlipidemia presented with intermittent conjunctival icterus for one year and recent pruritus. He denied prior liver disease and illicit drug use but admitted to drinking 3-4 drinks x 4 days/wk. Physical exam: Conjunctival icterus and mild jaundice. No ascites, xanthelasma, nail abnormalities, excoriations, telangiectasia, spider angioma, palmar erythema or peripheral edema noted. Initial labs shown in Table 1. Electrolytes, renal function, iron panel, HbA1c, TSH, aPTT, and INR were normal. HBV sAg-, HBV surface Ab+, HCV and HIV non-reactive. Patient declined abdominal ultrasound. Other labs revealed GGT 998, AFP 3.6, ANA 1:1280, IgA 553, IgG 3211, IgM 667, mitochondrial Ab 182.5, alpha-1-antitrypsin phenotype PI*MM, ceruloplasmin 46. Differential diagnosis included PBC vs autoimmune hepatitis (AIH). He was started on ursodeoxycholic acid (UDCA) 300 mg TID for cholestasis.
Liver biopsy revealed chronic lymphoplasmacytic portal hepatitis with ductopenia and bridging fibrosis, stage 3/4. Focal interface hepatitis with plasma cell clusters was present. The lobular parenchyma showed scattered lymphohistiocytic and plasma cell infiltrates along with pseudoduct formation and focal intracellular cholestasis. No steatosis or evidence of alcohol related injury. This confirmed the diagnosis of AIH and PBC. Azathioprine (AZA) 75 mg/day was started for presumed AIH.
One month later, he had fatigue, headaches, epigastric pain, and nausea with persistent conjunctival icterus and a new finding of muscle atrophy. He revealed he had not taken UDCA since pruritus was mild. AZA was titrated up to 100 mg/day and he was advised to take UDCA. The patient admitted taking high doses of turmeric for >1 year, prior to noting his off and on "yellow eyes". MRCP was consistent with PBC with a periportal halo sign with no evidence of primary sclerosing cholangitis.
Discussion: PBC is an autoimmune liver disease that predominantly affects women and is characterized by injury to small bile ducts. Several cases of turmeric-associated hepatocellular or cholestatic liver injury have been reported. This case presents the temporally related development of PBC/AIH after ingestion of a turmeric-containing supplement. Possible toxic effects of high dose turmeric need to be further investigated.
Disclosures:
Iqra Kazi indicated no relevant financial relationships.
Lisa Pedicone indicated no relevant financial relationships.
Jan Petrasek indicated no relevant financial relationships.
Carmen Landaverde indicated no relevant financial relationships.
Fabian Rodas indicated no relevant financial relationships.
Eugenia Tsai indicated no relevant financial relationships.
Eric Lawitz: 89Bio, Inc – Grant/Research Support. AbbVie – Grant/Research Support, Speakers Bureau. Akero – Advisor or Review Panel Member, Grant/Research Support. Allergan – Grant/Research Support. Alnylam – Grant/Research Support. Amgen – Grant/Research Support. Ascelia Pharma – Grant/Research Support. AstraZeneca – Grant/Research Support. Axcella Health – Grant/Research Support. Boehringer Ingelheim – Advisor or Review Panel Member, Grant/Research Support. Bristol Myers Squibb – Advisor or Review Panel Member, Grant/Research Support. Conatus Pharmaceuticals – Grant/Research Support. Cymabay – Grant/Research Support. CytoDyn – Grant/Research Support. DSM – Grant/Research Support. Durect Corporation – Grant/Research Support. Gilead – Speakers Bureau. Intercept – Advisor or Review Panel Member, Grant/Research Support, Speakers Bureau. Metacrine – Advisor or Review Panel Member. Novo Nordisk – Advisor or Review Panel Member. Sagimet – Advisor or Review Panel Member. Terns – Advisor or Review Panel Member.
Fred Poordad indicated no relevant financial relationships.
Iqra Kazi, MD1, Lisa Pedicone, PhD2, Jan Petrasek, MD, PhD3, Carmen Landaverde, MD4, Fabian Rodas, MD4, Eugenia Tsai, MD4, Eric Lawitz, MD4, Fred Poordad, MD4. P2519 - Rapidly Progressive Primary Biliary Cholangitis and Autoimmune Hepatitis Associated with Turmeric-Containing Supplements, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
