Monday Poster Session
Category: Liver
P2520 - Liver Transplantation in Biliary Papillomatosis of the Liver: Are We Going to Bell the Cat?
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Maya Mahmoud, MD
Saint Louis University
St. Louis, MO
Presenting Author(s)
Maya Mahmoud, MD, Michelle Baliss, DO, Kamran Qureshi, MD
Saint Louis University, St. Louis, MO
Introduction: Biliary papillomatosis (BP), also known as intraductal papillary neoplasm of the bile duct, is a rare premalignant entity characterized by bile duct epithelial cell proliferation leading to papillary tumors in the intrahepatic and extrahepatic bile ducts with high malignant potential and high recurrence rate following resection. The pathogenesis is poorly defined but is thought to be caused by chronic inflammation from recurrent infections or clonorchiasis. With extensive disease and liver involvement, radical resection with liver transplantation (LT) is the only potentially curative intervention.
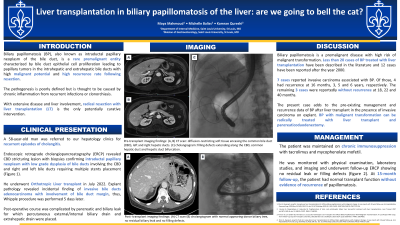
Case Description/Methods: We report the case of a 58-year-old man who was referred to our hepatology clinics for recurrent episodes of cholangitis. Endoscopic retrograde cholangiopancreatography (ERCP) revealed CBD stricturing lesion with biopsies confirming intraductal papillary neoplasm with low grade dysplasia of bile ducts involving the CBD and right and left bile ducts requiring multiple stents placement (A, B, C). He underwent Orthotropic LT in July 2022. Explant pathology revealed incidental finding of invasive bile ducts adenocarcinoma with involvement of bile duct margin, thus, Whipple procedure was performed 5 days later. Post-operative course was complicated by pancreatic and biliary leak for which percutaneous external/internal biliary drain and extrahepatic drain were placed. The patient was maintained on chronic immunosuppression with tacrolimus and mycophenolate mofetil. He was monitored with physical examination, laboratory studies, and imaging and underwent follow-up ERCP showing no residual leak or filling defects (D, E). At 12-month follow-up, the patient had normal transplant function without evidence of recurrence of papillomatosis.
Discussion: BP is a premalignant disease with high risk of malignant transformation. Less than 20 cases of BP treated with liver transplantation have been described in the literature and 12 cases have been reported after the year 2000. 7 cases reported invasive carcinoma associated with BP. Of those, 4 had recurrence at 16 months, 3, 5 and 6 years, respectively. The remaining 3 cases were reportedly without recurrence at 18, 22 and 40 months. The present case adds to the pre-existing management and recurrence data of BP after liver transplant in the presence of invasive carcinoma on explant. BP with malignant transformation can be radically treated with liver transplant and pancreaticoduodenectomy.

Disclosures:
Maya Mahmoud, MD, Michelle Baliss, DO, Kamran Qureshi, MD. P2520 - Liver Transplantation in Biliary Papillomatosis of the Liver: Are We Going to Bell the Cat?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Saint Louis University, St. Louis, MO
Introduction: Biliary papillomatosis (BP), also known as intraductal papillary neoplasm of the bile duct, is a rare premalignant entity characterized by bile duct epithelial cell proliferation leading to papillary tumors in the intrahepatic and extrahepatic bile ducts with high malignant potential and high recurrence rate following resection. The pathogenesis is poorly defined but is thought to be caused by chronic inflammation from recurrent infections or clonorchiasis. With extensive disease and liver involvement, radical resection with liver transplantation (LT) is the only potentially curative intervention.
Case Description/Methods: We report the case of a 58-year-old man who was referred to our hepatology clinics for recurrent episodes of cholangitis. Endoscopic retrograde cholangiopancreatography (ERCP) revealed CBD stricturing lesion with biopsies confirming intraductal papillary neoplasm with low grade dysplasia of bile ducts involving the CBD and right and left bile ducts requiring multiple stents placement (A, B, C). He underwent Orthotropic LT in July 2022. Explant pathology revealed incidental finding of invasive bile ducts adenocarcinoma with involvement of bile duct margin, thus, Whipple procedure was performed 5 days later. Post-operative course was complicated by pancreatic and biliary leak for which percutaneous external/internal biliary drain and extrahepatic drain were placed. The patient was maintained on chronic immunosuppression with tacrolimus and mycophenolate mofetil. He was monitored with physical examination, laboratory studies, and imaging and underwent follow-up ERCP showing no residual leak or filling defects (D, E). At 12-month follow-up, the patient had normal transplant function without evidence of recurrence of papillomatosis.
Discussion: BP is a premalignant disease with high risk of malignant transformation. Less than 20 cases of BP treated with liver transplantation have been described in the literature and 12 cases have been reported after the year 2000. 7 cases reported invasive carcinoma associated with BP. Of those, 4 had recurrence at 16 months, 3, 5 and 6 years, respectively. The remaining 3 cases were reportedly without recurrence at 18, 22 and 40 months. The present case adds to the pre-existing management and recurrence data of BP after liver transplant in the presence of invasive carcinoma on explant. BP with malignant transformation can be radically treated with liver transplant and pancreaticoduodenectomy.

Figure: (A, B) Pre-transplant computed tomography scan images showing diffusion-restricting soft tissue encasing the common bile duct (CBD), left and right hepatic ducts. (C) Pre-transplant cholangiogram showing filling defects extending along the CBD, common hepatic duct and hepatic duct bifurcation. (D, E) Post- transplant computed tomography scan and cholangiogram with normal appearing donor biliary tree, no residual biliary leak and no filling defects.
Disclosures:
Maya Mahmoud indicated no relevant financial relationships.
Michelle Baliss indicated no relevant financial relationships.
Kamran Qureshi: Gilead Sciences – Advisor or Review Panel Member, Speakers Bureau. Intercept Pharmaceuticals – Speakers Bureau. Salix Pharmaceuticals – Speakers Bureau.
Maya Mahmoud, MD, Michelle Baliss, DO, Kamran Qureshi, MD. P2520 - Liver Transplantation in Biliary Papillomatosis of the Liver: Are We Going to Bell the Cat?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
