Monday Poster Session
Category: Liver
P2553 - Hepatocellular Carcinoma Arising in a Non-Cirrhotic Patient With Hereditary Hemochromatosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Temitope Olasehinde, MD
Case Western Reserve University / University Hospitals
Cleveland, OH
Presenting Author(s)
Temitope Olasehinde, MD1, Adrian S. Lindsey, MD2, Anamay Sharma, MD3
1Case Western Reserve University / University Hospitals, Cleveland, OH; 2CWRU/UH/VA, Cleveland, OH; 3University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: It is well documented that the incidence of hepatocellular carcinoma (HCC) is markedly increased when chronic liver diseases, such as hereditary hemochromatosis (HH), advance to cirrhosis. However, less than 20% of HCC develops in the non-cirrhotic liver, with even less being reported as a result of HH. We report the rare case of a patient with HH who presented with HCC in the absence of liver cirrhosis.
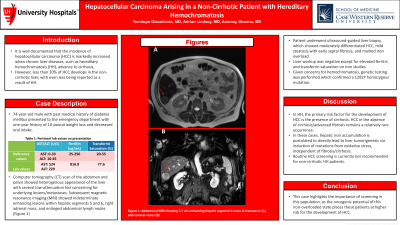
Case Description/Methods: A 74-year-old male with past medical history of diabetes mellitus presented to the emergency department with one-year history of 10-pound weight loss and decreased oral intake. Labs were significant for AST 524 U/L (reference: 0-33 U/L) and ALT 229 (reference: 10-45 U/L). Computer tomography (CT) scan of the abdomen and pelvis showed heterogenous appearance of the liver with several low-attenuation foci concerning for underlying lesions/metastases. Subsequent magnetic resonance imaging (MRI) showed indeterminate enhancing lesions within hepatic segments 5 and 6, right adrenal mass, and enlarged abdominal lymph nodes (Figure 1). Oncology was consulted, who recommended positron emission tomography (PET) scan, which showed no evidence of FDG avid malignancy/metastases. Patient underwent ultrasound-guided liver biopsy, which showed moderately differentiated HCC, mild steatosis with early septal fibrosis, and marked iron overload. Liver workup was negative, however, iron studies showed elevated ferritin to 816.8 ng/mL (reference: 25-250 ng/mL) and transferrin saturation of 77.6% (reference: 20-55%). Given concerns for hemochromatosis, genetic testing was performed which confirmed a C282Y homozygous mutation. Patient underwent ultrasound-guided microwave ablation of hepatic segments 5 and 6, and right adrenalectomy. He was diagnosed with stage IV HCC and was discharged with outpatient oncology follow-up for systemic treatment and phlebotomy.
Discussion: In HH, the primary risk factor for the development of HCC is the presence of cirrhosis. HCC in the absence of cirrhosis/advanced fibrosis remains a relatively rare occurrence. In these cases, hepatic iron accumulation is postulated to directly lead to liver tumorigenesis via induction of mutations from oxidative stress, independent of fibrosis/cirrhosis. Routine HCC screening is currently not recommended for non-cirrhotic HH patients. This case highlights the importance of screening in this population, as the oncogenic potential of this iron-overloaded state places these patients at higher risk for the development of HCC.

Disclosures:
Temitope Olasehinde, MD1, Adrian S. Lindsey, MD2, Anamay Sharma, MD3. P2553 - Hepatocellular Carcinoma Arising in a Non-Cirrhotic Patient With Hereditary Hemochromatosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Case Western Reserve University / University Hospitals, Cleveland, OH; 2CWRU/UH/VA, Cleveland, OH; 3University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: It is well documented that the incidence of hepatocellular carcinoma (HCC) is markedly increased when chronic liver diseases, such as hereditary hemochromatosis (HH), advance to cirrhosis. However, less than 20% of HCC develops in the non-cirrhotic liver, with even less being reported as a result of HH. We report the rare case of a patient with HH who presented with HCC in the absence of liver cirrhosis.
Case Description/Methods: A 74-year-old male with past medical history of diabetes mellitus presented to the emergency department with one-year history of 10-pound weight loss and decreased oral intake. Labs were significant for AST 524 U/L (reference: 0-33 U/L) and ALT 229 (reference: 10-45 U/L). Computer tomography (CT) scan of the abdomen and pelvis showed heterogenous appearance of the liver with several low-attenuation foci concerning for underlying lesions/metastases. Subsequent magnetic resonance imaging (MRI) showed indeterminate enhancing lesions within hepatic segments 5 and 6, right adrenal mass, and enlarged abdominal lymph nodes (Figure 1). Oncology was consulted, who recommended positron emission tomography (PET) scan, which showed no evidence of FDG avid malignancy/metastases. Patient underwent ultrasound-guided liver biopsy, which showed moderately differentiated HCC, mild steatosis with early septal fibrosis, and marked iron overload. Liver workup was negative, however, iron studies showed elevated ferritin to 816.8 ng/mL (reference: 25-250 ng/mL) and transferrin saturation of 77.6% (reference: 20-55%). Given concerns for hemochromatosis, genetic testing was performed which confirmed a C282Y homozygous mutation. Patient underwent ultrasound-guided microwave ablation of hepatic segments 5 and 6, and right adrenalectomy. He was diagnosed with stage IV HCC and was discharged with outpatient oncology follow-up for systemic treatment and phlebotomy.
Discussion: In HH, the primary risk factor for the development of HCC is the presence of cirrhosis. HCC in the absence of cirrhosis/advanced fibrosis remains a relatively rare occurrence. In these cases, hepatic iron accumulation is postulated to directly lead to liver tumorigenesis via induction of mutations from oxidative stress, independent of fibrosis/cirrhosis. Routine HCC screening is currently not recommended for non-cirrhotic HH patients. This case highlights the importance of screening in this population, as the oncogenic potential of this iron-overloaded state places these patients at higher risk for the development of HCC.

Figure: Figure 1: Abdominal MRI showing 3.7 cm enhancing hepatic segment 6 mass in transverse (A) and coronal views (B)
Disclosures:
Temitope Olasehinde indicated no relevant financial relationships.
Adrian Lindsey indicated no relevant financial relationships.
Anamay Sharma indicated no relevant financial relationships.
Temitope Olasehinde, MD1, Adrian S. Lindsey, MD2, Anamay Sharma, MD3. P2553 - Hepatocellular Carcinoma Arising in a Non-Cirrhotic Patient With Hereditary Hemochromatosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
