Monday Poster Session
Category: Liver
P2555 - Portal Hypertension: A Fluke?
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Michael Purviance, MD
San Joaquin General Hospital/ Internal Medicine
French Camp, CA
Presenting Author(s)
Michael Purviance, MD1, Anand Rajan, MD2, Marina Roytman, MD2
1San Joaquin General Hospital/ Internal Medicine, French Camp, CA; 2UCSF Fresno, Fresno, CA
Introduction: Schistosomiasis is endemic to over 78 countries around the world, with the World Health Organization estimating approximately 250 million who require treatment yearly [1]. There are six known common causative species of human schistosomiasis with five of the named species known as intestinal schistosomiasis, including S mekongi [2]. Acute infections of S mekongi can lead to hematochezia, diarrhea, constipation, and abdominal pain while chronic infections can lead to colonic ulcerations, polyposis, splenomegaly, and portal vein fibrosis [3]. Upper gastrointestinal bleeding (UGIB) is estimated to occur in 80% of people with chronic schistosomiasis and approximately 200 thousand people die per year in Sub-Saharan Africa from this complication alone [4]. Clinical suspicion in patients who are from endemic areas are important in order to provide early treatment to avoid catastrophic long term effects.
Case Description/Methods: 49-year-old man with alcohol related cirrhosis who presented with melena. Pertinent physical exam findings included diffuse abdominal tenderness and black tarry stool. Alkaline phosphatase 468 unit/L, ALT 12 unit/L, and AST 46 unit/L with a leukocytosis of 32,000 /uL. Emergent endoscopy revealed grade 1 esophageal varices and large volume of hematin in the fundus and body of the stomach without apparent site of active hemorrhage. Computerized tomography of the abdomen/pelvis was suggestive of cirrhotic morphology consistent with patient’s known alcohol cirrhosis.
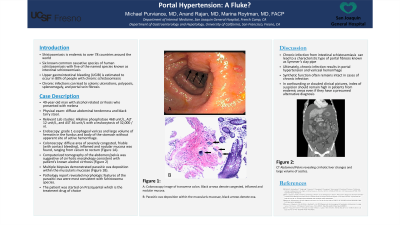
Colonoscopy showed a diffuse area of severely congested, friable (with contact bleeding), inflamed and nodular mucosa was found, ranging from cecum to rectum. Multiple biopsies were obtained and revealed parasitic ova deposition within the muscularis mucosae (Figure 1). The morphologic features of these ova were most consistent with Schistosoma species. The patient was started on Praziquantel which is the treatment drug of choice [5].
Discussion: Chronic infection from intestinal schistosomiasis, also known as Hepatosplenic schistosomiasis, can lead to a characteristic type of portal fibrosis called Symmer’s clay pipe or periportal fibrosis ultimately resulting in portal hypertension and variceal hemorrhage. As opposed to cirrhosis, synthetic function remains intact which is why in a confounding or clouded clinical picture, index of suspicion should remain high in patients from endemic areas even if they have a presumed alternative diagnosis.

Disclosures:
Michael Purviance, MD1, Anand Rajan, MD2, Marina Roytman, MD2. P2555 - Portal Hypertension: A Fluke?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1San Joaquin General Hospital/ Internal Medicine, French Camp, CA; 2UCSF Fresno, Fresno, CA
Introduction: Schistosomiasis is endemic to over 78 countries around the world, with the World Health Organization estimating approximately 250 million who require treatment yearly [1]. There are six known common causative species of human schistosomiasis with five of the named species known as intestinal schistosomiasis, including S mekongi [2]. Acute infections of S mekongi can lead to hematochezia, diarrhea, constipation, and abdominal pain while chronic infections can lead to colonic ulcerations, polyposis, splenomegaly, and portal vein fibrosis [3]. Upper gastrointestinal bleeding (UGIB) is estimated to occur in 80% of people with chronic schistosomiasis and approximately 200 thousand people die per year in Sub-Saharan Africa from this complication alone [4]. Clinical suspicion in patients who are from endemic areas are important in order to provide early treatment to avoid catastrophic long term effects.
Case Description/Methods: 49-year-old man with alcohol related cirrhosis who presented with melena. Pertinent physical exam findings included diffuse abdominal tenderness and black tarry stool. Alkaline phosphatase 468 unit/L, ALT 12 unit/L, and AST 46 unit/L with a leukocytosis of 32,000 /uL. Emergent endoscopy revealed grade 1 esophageal varices and large volume of hematin in the fundus and body of the stomach without apparent site of active hemorrhage. Computerized tomography of the abdomen/pelvis was suggestive of cirrhotic morphology consistent with patient’s known alcohol cirrhosis.
Colonoscopy showed a diffuse area of severely congested, friable (with contact bleeding), inflamed and nodular mucosa was found, ranging from cecum to rectum. Multiple biopsies were obtained and revealed parasitic ova deposition within the muscularis mucosae (Figure 1). The morphologic features of these ova were most consistent with Schistosoma species. The patient was started on Praziquantel which is the treatment drug of choice [5].
Discussion: Chronic infection from intestinal schistosomiasis, also known as Hepatosplenic schistosomiasis, can lead to a characteristic type of portal fibrosis called Symmer’s clay pipe or periportal fibrosis ultimately resulting in portal hypertension and variceal hemorrhage. As opposed to cirrhosis, synthetic function remains intact which is why in a confounding or clouded clinical picture, index of suspicion should remain high in patients from endemic areas even if they have a presumed alternative diagnosis.

Figure: Figure 1: Cecum Biopsy with black arrows denoting Schistosoma ova.
Disclosures:
Michael Purviance indicated no relevant financial relationships.
Anand Rajan indicated no relevant financial relationships.
Marina Roytman: Gilead – Advisor or Review Panel Member. Intercept – Advisor or Review Panel Member. VBI – Advisor or Review Panel Member.
Michael Purviance, MD1, Anand Rajan, MD2, Marina Roytman, MD2. P2555 - Portal Hypertension: A Fluke?, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
