Monday Poster Session
Category: Liver
P2556 - Post COVID-19 Cholangiopathy: An Emerging Entity
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Muaaz Masood, MD
Virginia Mason Franciscan Health
Seattle, WA
Presenting Author(s)
Muaaz Masood, MD, Erin Forsythe, ARNP, Asma Siddique, MD, Blaire Burman, MD, Rajesh Krishnamoorthi, MD
Virginia Mason Franciscan Health, Seattle, WA
Introduction: Post-COVID-19 cholangiopathy (PCC) is a rare, but severe and emerging complication of COVID-19 that can occur weeks to months following COVID-19. Patients with COVID-19 and abnormal liver enzymes, especially in a cholestatic pattern, have poor outcomes and an increased mortality.
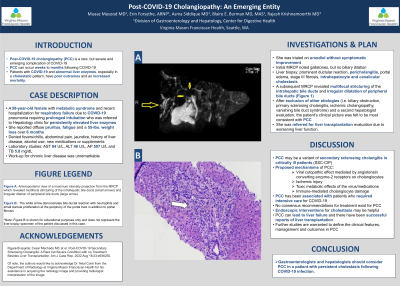
Case Description/Methods: A 58-year-old female with metabolic syndrome and recent hospitalization for respiratory failure due to COVID-19 pneumonia requiring prolonged intubation who was referred to Hepatology clinic for persistently elevated liver enzymes. She reported diffuse pruritus, fatigue and a 55-lbs. weight loss over 6 months. The patient denied fevers/chills, abdominal pain, jaundice, history of liver disease, alcohol use, new medications or supplements. Laboratory studies revealed AST 84 U/L, ALT 46 U/L, AP 597 U/L and TB 5.8 mg/dL. Work-up for chronic liver disease was unremarkable. She was trialed on ursodiol without symptomatic improvement. Initial MRCP noted gallstones, but no biliary dilation. Liver biopsy was obtained and demonstrated prominent ductular reaction, pericholangitis, portal edema, stage III fibrosis, intrahepatocyte and canalicular cholestasis. A subsequent MRCP revealed multifocal stricturing of the intrahepatic bile ducts and irregular dilatation of peripheral bile ducts (Figure 1). After exclusion of other etiologies (i.e. biliary obstruction, primary sclerosing cholangitis, ischemic cholangiopathy, vanishing bile duct syndrome) and a second hepatologist evaluation, the patient’s clinical picture was felt to be most consistent with PCC. She was referred for liver transplantation evaluation due to worsening liver function.
Discussion: PCC may be a variant of secondary sclerosing cholangitis in critically ill patients (SSC-CIP). Proposed mechanisms of PCC include viral cytopathic effect mediated by angiotensin converting enzyme-2 receptors on cholangiocytes, ischemic injury, toxic metabolic effects of the virus/medications and immune-mediated cholangiocyte damage. PCC has been associated with patients who required intensive care for COVID-19. No consensus recommendations for treatment exist for PCC. Endoscopic interventions for cholestasis may be helpful. PCC can lead to liver failure and there have been successful reports of liver transplantation. Further studies are warranted to define the clinical features, management and outcomes in PCC. Gastroenterologists and hepatologists should consider PCC in a patient with persistent cholestasis following COVID-19 infection.

Disclosures:
Muaaz Masood, MD, Erin Forsythe, ARNP, Asma Siddique, MD, Blaire Burman, MD, Rajesh Krishnamoorthi, MD. P2556 - Post COVID-19 Cholangiopathy: An Emerging Entity, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Virginia Mason Franciscan Health, Seattle, WA
Introduction: Post-COVID-19 cholangiopathy (PCC) is a rare, but severe and emerging complication of COVID-19 that can occur weeks to months following COVID-19. Patients with COVID-19 and abnormal liver enzymes, especially in a cholestatic pattern, have poor outcomes and an increased mortality.
Case Description/Methods: A 58-year-old female with metabolic syndrome and recent hospitalization for respiratory failure due to COVID-19 pneumonia requiring prolonged intubation who was referred to Hepatology clinic for persistently elevated liver enzymes. She reported diffuse pruritus, fatigue and a 55-lbs. weight loss over 6 months. The patient denied fevers/chills, abdominal pain, jaundice, history of liver disease, alcohol use, new medications or supplements. Laboratory studies revealed AST 84 U/L, ALT 46 U/L, AP 597 U/L and TB 5.8 mg/dL. Work-up for chronic liver disease was unremarkable. She was trialed on ursodiol without symptomatic improvement. Initial MRCP noted gallstones, but no biliary dilation. Liver biopsy was obtained and demonstrated prominent ductular reaction, pericholangitis, portal edema, stage III fibrosis, intrahepatocyte and canalicular cholestasis. A subsequent MRCP revealed multifocal stricturing of the intrahepatic bile ducts and irregular dilatation of peripheral bile ducts (Figure 1). After exclusion of other etiologies (i.e. biliary obstruction, primary sclerosing cholangitis, ischemic cholangiopathy, vanishing bile duct syndrome) and a second hepatologist evaluation, the patient’s clinical picture was felt to be most consistent with PCC. She was referred for liver transplantation evaluation due to worsening liver function.
Discussion: PCC may be a variant of secondary sclerosing cholangitis in critically ill patients (SSC-CIP). Proposed mechanisms of PCC include viral cytopathic effect mediated by angiotensin converting enzyme-2 receptors on cholangiocytes, ischemic injury, toxic metabolic effects of the virus/medications and immune-mediated cholangiocyte damage. PCC has been associated with patients who required intensive care for COVID-19. No consensus recommendations for treatment exist for PCC. Endoscopic interventions for cholestasis may be helpful. PCC can lead to liver failure and there have been successful reports of liver transplantation. Further studies are warranted to define the clinical features, management and outcomes in PCC. Gastroenterologists and hepatologists should consider PCC in a patient with persistent cholestasis following COVID-19 infection.

Figure: Figure 1. Anteroposterior view of a maximum intensity projection from the magnetic resonance cholangiopancreatography which revealed multifocal stricturing of the intrahepatic bile ducts (small arrows) and irregular dilation of peripheral bile ducts (large arrow). Of note, the authors would like to acknowledge Dr. Neal Conti from the Department of Radiology at Virginia Mason Franciscan Health for his assistance in acquiring the radiology image and providing radiologist interpretation of the image.
Disclosures:
Muaaz Masood indicated no relevant financial relationships.
Erin Forsythe indicated no relevant financial relationships.
Asma Siddique indicated no relevant financial relationships.
Blaire Burman indicated no relevant financial relationships.
Rajesh Krishnamoorthi indicated no relevant financial relationships.
Muaaz Masood, MD, Erin Forsythe, ARNP, Asma Siddique, MD, Blaire Burman, MD, Rajesh Krishnamoorthi, MD. P2556 - Post COVID-19 Cholangiopathy: An Emerging Entity, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

