Monday Poster Session
Category: Liver
P2557 - Hepatic Hydatid Cyst With a Negative Serology
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Muaaz Masood, MD
Virginia Mason Franciscan Health
Seattle, WA
Presenting Author(s)
Muaaz Masood, MD1, Asma Siddique, MD1, Rajesh Krishnamoorthi, MD1, Blaire Burman, MD1, Richard Kozarek, MD, FACG2
1Virginia Mason Franciscan Health, Seattle, WA; 2Virginia Mason Franciscan Health/Benaroya Research Institute, Seattle, WA
Introduction: Hydatid cysts (HC) are caused by the larvae of the tapeworm Echinococcus granulosus found in infected dogs, sheep, cattle, goats and pigs. Humans become infected by the ingestion of parasite eggs found in contaminated food or after direct contact with the host animals. While HC are rare in the United States, HC may be seen in immigrants from and travelers to endemic areas. HC most commonly affects the liver and may be life-threatening.
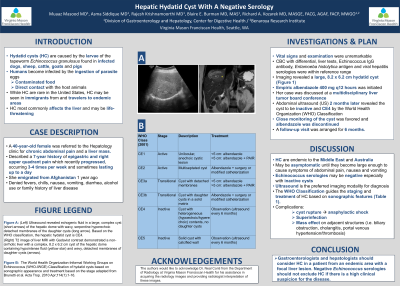
Case Description/Methods: A 40-year-old female was referred to the Hepatology clinic for chronic abdominal pain and a liver mass. She described a 7-year history of epigastric and right upper quadrant pain which recently progressed, occurring 3-4 times per week and sometimes lasting up to a day. She emigrated from Afghanistan 1 year ago. The patient denied fevers, chills, nausea, vomiting, diarrhea, alcohol use or family history of liver disease. Vital signs and examination were unremarkable. A complete blood count with differential, liver function tests, Echinococcus IgG antibody, Entamoeba histolytica antigen and acute viral hepatitis serologies were within reference range. Imaging revealed a large, 8.2 x 6.2 cm hydatid cyst (Figure 1). Empiric albendazole 400 mg q12 hours was initiated and her case was discussed at a multidisciplinary liver tumor board conference. Abdominal ultrasound (US) 2 months later revealed the cyst to be inactive and CE4 by the World Health Organization (WHO) Classification. Close monitoring of the cyst was favored and albendazole was discontinued. A follow-up visit was arranged for 6 months.
Discussion: HC are endemic to the Middle East and Australia and may be asymptomatic for years until they become large enough to cause symptoms of abdominal pain, nausea and vomiting. It is important to note that Echinococcus serologies may be negative especially with inactive cysts. US is the preferred imaging modality for diagnosis though MRI/CT are often also obtained for a comprehensive evaluation. The WHO Classification guides the staging and treatment of HC based on sonographic features (Table 1). Complications include cyst rupture leading to anaphylactic shock, superinfection and mass effect on adjacent structures (i.e. biliary obstruction, cholangitis, portal venous hypertension/thrombosis). Gastroenterologists and hepatologists should consider HC in a patient from an endemic area with a focal liver lesion. Negative Echinococcus serologies should not exclude HC if there is a high clinical suspicion for the disease.

Disclosures:
Muaaz Masood, MD1, Asma Siddique, MD1, Rajesh Krishnamoorthi, MD1, Blaire Burman, MD1, Richard Kozarek, MD, FACG2. P2557 - Hepatic Hydatid Cyst With a Negative Serology, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Virginia Mason Franciscan Health, Seattle, WA; 2Virginia Mason Franciscan Health/Benaroya Research Institute, Seattle, WA
Introduction: Hydatid cysts (HC) are caused by the larvae of the tapeworm Echinococcus granulosus found in infected dogs, sheep, cattle, goats and pigs. Humans become infected by the ingestion of parasite eggs found in contaminated food or after direct contact with the host animals. While HC are rare in the United States, HC may be seen in immigrants from and travelers to endemic areas. HC most commonly affects the liver and may be life-threatening.
Case Description/Methods: A 40-year-old female was referred to the Hepatology clinic for chronic abdominal pain and a liver mass. She described a 7-year history of epigastric and right upper quadrant pain which recently progressed, occurring 3-4 times per week and sometimes lasting up to a day. She emigrated from Afghanistan 1 year ago. The patient denied fevers, chills, nausea, vomiting, diarrhea, alcohol use or family history of liver disease. Vital signs and examination were unremarkable. A complete blood count with differential, liver function tests, Echinococcus IgG antibody, Entamoeba histolytica antigen and acute viral hepatitis serologies were within reference range. Imaging revealed a large, 8.2 x 6.2 cm hydatid cyst (Figure 1). Empiric albendazole 400 mg q12 hours was initiated and her case was discussed at a multidisciplinary liver tumor board conference. Abdominal ultrasound (US) 2 months later revealed the cyst to be inactive and CE4 by the World Health Organization (WHO) Classification. Close monitoring of the cyst was favored and albendazole was discontinued. A follow-up visit was arranged for 6 months.
Discussion: HC are endemic to the Middle East and Australia and may be asymptomatic for years until they become large enough to cause symptoms of abdominal pain, nausea and vomiting. It is important to note that Echinococcus serologies may be negative especially with inactive cysts. US is the preferred imaging modality for diagnosis though MRI/CT are often also obtained for a comprehensive evaluation. The WHO Classification guides the staging and treatment of HC based on sonographic features (Table 1). Complications include cyst rupture leading to anaphylactic shock, superinfection and mass effect on adjacent structures (i.e. biliary obstruction, cholangitis, portal venous hypertension/thrombosis). Gastroenterologists and hepatologists should consider HC in a patient from an endemic area with a focal liver lesion. Negative Echinococcus serologies should not exclude HC if there is a high clinical suspicion for the disease.

Figure: Figure 1. (Left) Ultrasound revealed echogenic fluid in a large, complex cyst (short arrows) of the hepatic dome with wavy, serpentine hyperechoic detached membranes of the daughter cysts (long arrow). Etiology is most consistent with a hydatid cyst. Based on the WHO classification, the hepatic hydatid cyst is CE4. (Right) T2 image of the magnetic resonance imaging of the liver with Gadavist contrast demonstrated a non-cirrhotic liver with a complex, 8.2 x 6.2 cm cyst of the hepatic dome containing hypointense fluid (yellow star) and wavy, detached membranes of daughter cysts (arrows). Of note, the authors would like to acknowledge Dr. Neal Conti from the Department of Radiology at Virginia Mason Franciscan Health for his assistance in acquiring the radiology images and providing radiologist interpretation of these images.
Disclosures:
Muaaz Masood indicated no relevant financial relationships.
Asma Siddique indicated no relevant financial relationships.
Rajesh Krishnamoorthi indicated no relevant financial relationships.
Blaire Burman indicated no relevant financial relationships.
Richard Kozarek indicated no relevant financial relationships.
Muaaz Masood, MD1, Asma Siddique, MD1, Rajesh Krishnamoorthi, MD1, Blaire Burman, MD1, Richard Kozarek, MD, FACG2. P2557 - Hepatic Hydatid Cyst With a Negative Serology, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
