Monday Poster Session
Category: Liver
P2558 - Congenital Hepatic Fibrosis in Adulthood
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Muaaz Masood, MD
Virginia Mason Franciscan Health
Seattle, WA
Presenting Author(s)
Muaaz Masood, MD1, Richard Kozarek, MD, FACG2, Blaire Burman, MD1, Rajesh Krishnamoorthi, MD1, Asma Siddique, MD1
1Virginia Mason Franciscan Health, Seattle, WA; 2Virginia Mason Franciscan Health/Benaroya Research Institute, Seattle, WA
Introduction: Congenital hepatic fibrosis (CHF) is a rare, autosomal recessive, fibropolycystic disease which occurs due ductal plate malformation and is associated with several inherited syndromes i.e. Caroli disease and polycystic kidney disease. While CHF is commonly diagnosed in childhood, it may present in adults as late as age 40-50. Clinical presentation is often variable which can pose a challenge for diagnosis.
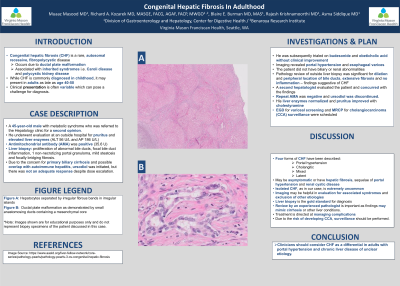
Case Description/Methods: A 45-year-old male with metabolic syndrome who was referred to the Hepatology clinic for a second opinion. He underwent evaluation at an outside hospital for pruritus and elevated liver enzymes with ALT 56 U/L and AP 186 U/L. Antimitochondrial antibody (AMA) was positive at 35.6 U. Liver biopsy noted proliferation of abnormal bile ducts, focal bile duct inflammation, single non-necrotizing portal granuloma, mild steatosis and focally bridging fibrosis. Due to the concern for primary biliary cirrhosis and possible overlap with autoimmune hepatitis, ursodiol was initiated, but there was not an adequate response despite dose escalation. He was subsequently trialed on budesonide and obeticholic acid without clinical improvement. Imaging revealed portal hypertension and esophageal varices. The patient did not have biliary or renal abnormalities. Pathology review of outside liver biopsy was significant for dilation and peripheral location of bile ducts, extensive fibrosis and no inflammation – findings suggestive of CHF. A second hepatologist evaluated the patient and concurred with the findings. Repeat AMA was negative and ursodiol was discontinued. His liver enzymes normalized and pruritus improved with cholestyramine. EGD for variceal screening and MRCP for cholangiocarcinoma (CCA) surveillance were scheduled.
Discussion: Four forms of CHF have been described: portal hypertension, cholangitic, mixed and latent. Patients may be asymptomatic or have hepatic fibrosis, sequelae of portal hypertension and renal cystic disease. Isolated CHF, as in our case, is extremely uncommon. Imaging may be helpful in evaluation for associated syndromes and exclusion of other etiologies. Liver biopsy is the gold standard for diagnosis. Review by an experienced pathologist is important as findings may mimic cirrhosis or other liver conditions. Treatment is directed at managing complications. Due to the risk of developing CCA, surveillance should be performed. Clinicians should consider CHF as a differential in adults with portal hypertension and chronic liver disease of unclear etiology.
Disclosures:
Muaaz Masood, MD1, Richard Kozarek, MD, FACG2, Blaire Burman, MD1, Rajesh Krishnamoorthi, MD1, Asma Siddique, MD1. P2558 - Congenital Hepatic Fibrosis in Adulthood, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Virginia Mason Franciscan Health, Seattle, WA; 2Virginia Mason Franciscan Health/Benaroya Research Institute, Seattle, WA
Introduction: Congenital hepatic fibrosis (CHF) is a rare, autosomal recessive, fibropolycystic disease which occurs due ductal plate malformation and is associated with several inherited syndromes i.e. Caroli disease and polycystic kidney disease. While CHF is commonly diagnosed in childhood, it may present in adults as late as age 40-50. Clinical presentation is often variable which can pose a challenge for diagnosis.
Case Description/Methods: A 45-year-old male with metabolic syndrome who was referred to the Hepatology clinic for a second opinion. He underwent evaluation at an outside hospital for pruritus and elevated liver enzymes with ALT 56 U/L and AP 186 U/L. Antimitochondrial antibody (AMA) was positive at 35.6 U. Liver biopsy noted proliferation of abnormal bile ducts, focal bile duct inflammation, single non-necrotizing portal granuloma, mild steatosis and focally bridging fibrosis. Due to the concern for primary biliary cirrhosis and possible overlap with autoimmune hepatitis, ursodiol was initiated, but there was not an adequate response despite dose escalation. He was subsequently trialed on budesonide and obeticholic acid without clinical improvement. Imaging revealed portal hypertension and esophageal varices. The patient did not have biliary or renal abnormalities. Pathology review of outside liver biopsy was significant for dilation and peripheral location of bile ducts, extensive fibrosis and no inflammation – findings suggestive of CHF. A second hepatologist evaluated the patient and concurred with the findings. Repeat AMA was negative and ursodiol was discontinued. His liver enzymes normalized and pruritus improved with cholestyramine. EGD for variceal screening and MRCP for cholangiocarcinoma (CCA) surveillance were scheduled.
Discussion: Four forms of CHF have been described: portal hypertension, cholangitic, mixed and latent. Patients may be asymptomatic or have hepatic fibrosis, sequelae of portal hypertension and renal cystic disease. Isolated CHF, as in our case, is extremely uncommon. Imaging may be helpful in evaluation for associated syndromes and exclusion of other etiologies. Liver biopsy is the gold standard for diagnosis. Review by an experienced pathologist is important as findings may mimic cirrhosis or other liver conditions. Treatment is directed at managing complications. Due to the risk of developing CCA, surveillance should be performed. Clinicians should consider CHF as a differential in adults with portal hypertension and chronic liver disease of unclear etiology.
Disclosures:
Muaaz Masood indicated no relevant financial relationships.
Richard Kozarek indicated no relevant financial relationships.
Blaire Burman indicated no relevant financial relationships.
Rajesh Krishnamoorthi indicated no relevant financial relationships.
Asma Siddique indicated no relevant financial relationships.
Muaaz Masood, MD1, Richard Kozarek, MD, FACG2, Blaire Burman, MD1, Rajesh Krishnamoorthi, MD1, Asma Siddique, MD1. P2558 - Congenital Hepatic Fibrosis in Adulthood, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
