Monday Poster Session
Category: Liver
P2561 - Lipoprotein X Syndrome: A Consideration for Liver Transplant in Primary Sclerosing Cholangitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Lauren Shaffer, MD
University of Pennsylvania
Philadelphia, PA
Presenting Author(s)
Lauren Shaffer, MD, Daniel Soffer, MD, Stacey Prenner, MD
University of Pennsylvania, Philadelphia, PA
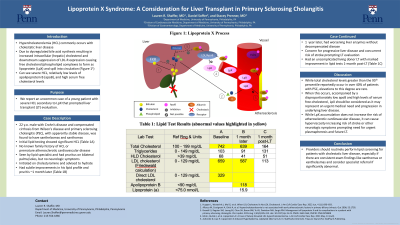
Introduction: Hypercholesterolemia (HCL) commonly occurs in patients with cholestatic liver disease. This occurs due to impaired low-density lipoprotein-receptor (LDL-R) expression and late developing increase in lipoprotein-X (LpX). Cholestasis causes dysregulated bile acid synthesis resulting in increased intracellular (hepatic) cholesterol and downstream suppression of LDL-R expression. As the disease progresses, free cholesterol/phospholipid complexes form as LpX and spill into the circulation. This is characterized by acquired severe HCL in the right clinical context. We report an uncommon case of a young patient with severe HCL secondary to LpX that prompted liver transplant (LT) evaluation.
Case Description/Methods: A 22 y.o. male with Crohn’s disease and compensated cirrhosis from Wilson’s disease and primary sclerosing cholangitis (PSC), with apparently stable disease on mesalamine, trientine, and ursodiol, visited an ophthalmologist to discuss yellow growths on his eyelids. He was sent for first-time lipid testing that showed significant HCL (Table 1A) prompting referral to a lipid specialist. He had no family history of HCL or premature atherosclerotic cardiovascular disease (ASCVD). During that visit, he had findings of eyelid xanthelasmas and xanthomas on bilateral palms/soles with associated pruritus, but no neurologic symptoms. He was initiated on cholestyramine and advised to hydrate. He had subtle improvements in his lipid profile and pruritis three weeks later (Table 1B). One year later, the patient had worsening liver enzymes without decompensated disease. The concern for progressive liver disease and concurrent risk of stroke from hyperviscosity secondary to LpX syndrome prompted LT evaluation. The patient ultimately had an uncomplicated living donor LT with marked improvement in his lipid profile one month post-LT (Table 1C).
Discussion: While total cholesterol levels greater than the 95th percentile reportedly occur in over 40% of patients with PSC, elevations to this degree are rare. When this occurs, LpX should be considered as it may represent an urgent medical need and progression in underlying liver disease. While LpX accumulation does not increase the risk of ASCVD, it can cause hyperviscosity increasing risk of stroke or other neurologic symptoms prompting need for urgent plasmapheresis and future LT. Providers should routinely perform lipid screening for patients with cholestatic liver disease, especially if there are consistent exam findings like xanthomas or xanthelasmas.
Disclosures:
Lauren Shaffer, MD, Daniel Soffer, MD, Stacey Prenner, MD. P2561 - Lipoprotein X Syndrome: A Consideration for Liver Transplant in Primary Sclerosing Cholangitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Pennsylvania, Philadelphia, PA
Introduction: Hypercholesterolemia (HCL) commonly occurs in patients with cholestatic liver disease. This occurs due to impaired low-density lipoprotein-receptor (LDL-R) expression and late developing increase in lipoprotein-X (LpX). Cholestasis causes dysregulated bile acid synthesis resulting in increased intracellular (hepatic) cholesterol and downstream suppression of LDL-R expression. As the disease progresses, free cholesterol/phospholipid complexes form as LpX and spill into the circulation. This is characterized by acquired severe HCL in the right clinical context. We report an uncommon case of a young patient with severe HCL secondary to LpX that prompted liver transplant (LT) evaluation.
Case Description/Methods: A 22 y.o. male with Crohn’s disease and compensated cirrhosis from Wilson’s disease and primary sclerosing cholangitis (PSC), with apparently stable disease on mesalamine, trientine, and ursodiol, visited an ophthalmologist to discuss yellow growths on his eyelids. He was sent for first-time lipid testing that showed significant HCL (Table 1A) prompting referral to a lipid specialist. He had no family history of HCL or premature atherosclerotic cardiovascular disease (ASCVD). During that visit, he had findings of eyelid xanthelasmas and xanthomas on bilateral palms/soles with associated pruritus, but no neurologic symptoms. He was initiated on cholestyramine and advised to hydrate. He had subtle improvements in his lipid profile and pruritis three weeks later (Table 1B). One year later, the patient had worsening liver enzymes without decompensated disease. The concern for progressive liver disease and concurrent risk of stroke from hyperviscosity secondary to LpX syndrome prompted LT evaluation. The patient ultimately had an uncomplicated living donor LT with marked improvement in his lipid profile one month post-LT (Table 1C).
Discussion: While total cholesterol levels greater than the 95th percentile reportedly occur in over 40% of patients with PSC, elevations to this degree are rare. When this occurs, LpX should be considered as it may represent an urgent medical need and progression in underlying liver disease. While LpX accumulation does not increase the risk of ASCVD, it can cause hyperviscosity increasing risk of stroke or other neurologic symptoms prompting need for urgent plasmapheresis and future LT. Providers should routinely perform lipid screening for patients with cholestatic liver disease, especially if there are consistent exam findings like xanthomas or xanthelasmas.
Disclosures:
Lauren Shaffer indicated no relevant financial relationships.
Daniel Soffer: Akcea – Consultant. Amgen Inc – investigator, data monitoring. Amryt – investigator. Astra-Zeneca – Investigator. Ionis – investigator. Novartis – Consultant, writing support. Regeneron – Consultant. RegenXBio – investigator. Verve Therapeutics – Investigator.
Stacey Prenner indicated no relevant financial relationships.
Lauren Shaffer, MD, Daniel Soffer, MD, Stacey Prenner, MD. P2561 - Lipoprotein X Syndrome: A Consideration for Liver Transplant in Primary Sclerosing Cholangitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
