Monday Poster Session
Category: Liver
P2562 - Recurrent Pyogenic Liver Abscess – An Indication for Cancer Screening
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Andrew Krane, MD
Warren Alpert Medical School of Brown University
Providence, RI
Presenting Author(s)
Andrew Krane, MD1, Suvithan Rajadurai, MD1, Samir A. Shah, MD, FACG2
1Warren Alpert Medical School of Brown University, Providence, RI; 2Gastroenterology Associates, Inc., Providence, RI
Introduction: In current literature, there appears to be an association between colon cancer, hepatobiliary malignancies, and pyogenic liver abscesses (PLA). Most often, these infections are polymicrobial, but may grow specific organisms which may indicate a more probable source of underlying malignancy. Here we present a case of recurrent polymicrobial PLA presenting initially as acute hypoxic respiratory failure.
Case Description/Methods: A 53-year-old male with Down syndrome and newly diagnosed PLAs presents to the hospital in acute hypoxic respiratory failure with complaints of shortness of breath, fevers and chills. Of note, he was admitted one month prior and had a hepatic drain placed with an extended course of antibiotics. Vital signs were notable for a blood pressure of 80/60 mmHg and oxygen saturation of 70% on room air. On physical exam, he is in distress with right upper quadrant tenderness to palpation and decreased breath sounds of the right lung. Abdominal computed tomography (CT) imaging was obtained and revealed stable hepatic abscesses (Figure 1, A). Laboratory studies were notable for ALP 900 U/L, AST 64 U/L, ALT 42 U/L, Total bilirubin of 0.4mg/dL. He was transferred to the ICU and treated for a parapneumonic effusion with drainage via chest tube placement and 7 days of antibiotic therapy. Upon completion of antibiotics, he clinically decompensated with a rising leukocytosis prompting new CT and MRI imaging. Interval imaging revealed new scattered hepatic lesions concerning for abscesses, as well as a loculated peritoneal fluid concerning for infection (Figure 1, B-D). Further serologic testing revealed a CA 19-9 of 422,639 U/mL and CEA 11ug/L. He underwent paracentesis with pathology revealing adenocarcinoma of unknown primary source with stains positive for MOC-31, Cytokeratin 7, and Cytokeratin 903. The patient was transitioned to hospice on discharge with therapeutic paracenteses for comfort.
Discussion: Prompt evaluation and drainage of PLAs is key to treatment, but also, diagnosis of an underlying source is paramount to prevent recurrences or complications. Common mechanisms of PLA development include ascending biliary or intraperitoneal infection, portal bacteremia, direct liver trauma, or infection from cancer. Our patient likely had a pancreaticobiliary source of malignancy leading to recurrent bacterial translocation into splanchnic circulation. In cases of cryptogenic pyogenic liver abscesses, screening for underlying hepatobiliary or colonic malignancies is warranted.

Disclosures:
Andrew Krane, MD1, Suvithan Rajadurai, MD1, Samir A. Shah, MD, FACG2. P2562 - Recurrent Pyogenic Liver Abscess – An Indication for Cancer Screening, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Warren Alpert Medical School of Brown University, Providence, RI; 2Gastroenterology Associates, Inc., Providence, RI
Introduction: In current literature, there appears to be an association between colon cancer, hepatobiliary malignancies, and pyogenic liver abscesses (PLA). Most often, these infections are polymicrobial, but may grow specific organisms which may indicate a more probable source of underlying malignancy. Here we present a case of recurrent polymicrobial PLA presenting initially as acute hypoxic respiratory failure.
Case Description/Methods: A 53-year-old male with Down syndrome and newly diagnosed PLAs presents to the hospital in acute hypoxic respiratory failure with complaints of shortness of breath, fevers and chills. Of note, he was admitted one month prior and had a hepatic drain placed with an extended course of antibiotics. Vital signs were notable for a blood pressure of 80/60 mmHg and oxygen saturation of 70% on room air. On physical exam, he is in distress with right upper quadrant tenderness to palpation and decreased breath sounds of the right lung. Abdominal computed tomography (CT) imaging was obtained and revealed stable hepatic abscesses (Figure 1, A). Laboratory studies were notable for ALP 900 U/L, AST 64 U/L, ALT 42 U/L, Total bilirubin of 0.4mg/dL. He was transferred to the ICU and treated for a parapneumonic effusion with drainage via chest tube placement and 7 days of antibiotic therapy. Upon completion of antibiotics, he clinically decompensated with a rising leukocytosis prompting new CT and MRI imaging. Interval imaging revealed new scattered hepatic lesions concerning for abscesses, as well as a loculated peritoneal fluid concerning for infection (Figure 1, B-D). Further serologic testing revealed a CA 19-9 of 422,639 U/mL and CEA 11ug/L. He underwent paracentesis with pathology revealing adenocarcinoma of unknown primary source with stains positive for MOC-31, Cytokeratin 7, and Cytokeratin 903. The patient was transitioned to hospice on discharge with therapeutic paracenteses for comfort.
Discussion: Prompt evaluation and drainage of PLAs is key to treatment, but also, diagnosis of an underlying source is paramount to prevent recurrences or complications. Common mechanisms of PLA development include ascending biliary or intraperitoneal infection, portal bacteremia, direct liver trauma, or infection from cancer. Our patient likely had a pancreaticobiliary source of malignancy leading to recurrent bacterial translocation into splanchnic circulation. In cases of cryptogenic pyogenic liver abscesses, screening for underlying hepatobiliary or colonic malignancies is warranted.

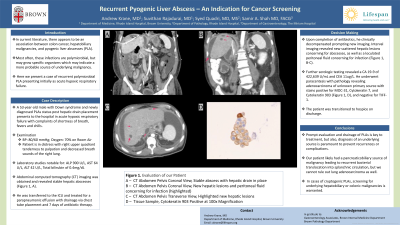
Figure: Figure 1: Evaluation of our Patient
A – CT Abdomen Pelvis Coronal View - Stable abscess with hepatic drain in place
B – CT Abdomen Pelvis Coronal View - New hepatic lesions and peritoneal fluid concerning for infection (highlighted)
C – CT Abdomen Pelvis Transverse View - Highlighted new hepatic lesions
D – MRI Abdomen T2 Weighted - Dimensions of largest abscess
A – CT Abdomen Pelvis Coronal View - Stable abscess with hepatic drain in place
B – CT Abdomen Pelvis Coronal View - New hepatic lesions and peritoneal fluid concerning for infection (highlighted)
C – CT Abdomen Pelvis Transverse View - Highlighted new hepatic lesions
D – MRI Abdomen T2 Weighted - Dimensions of largest abscess
Disclosures:
Andrew Krane indicated no relevant financial relationships.
Suvithan Rajadurai indicated no relevant financial relationships.
Samir Shah indicated no relevant financial relationships.
Andrew Krane, MD1, Suvithan Rajadurai, MD1, Samir A. Shah, MD, FACG2. P2562 - Recurrent Pyogenic Liver Abscess – An Indication for Cancer Screening, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
