Monday Poster Session
Category: Liver
P2568 - A Rare Case of Drug-Induced Immune Thrombocytopenia From Hepatocellular Carcinoma Treatment
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- AS
Avneet Singh, DO
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Avneet Singh, DO, Alexander Garcia, DO, Ishita Dhawan, MD, Tara Lautenslager, MD
Cooper University Hospital, Camden, NJ
Introduction: Atezolizumab is an immune checkpoint inhibitor that binds PD-L1 and bevacizumab is an antiangiogenic that are considered a standard of care in patients with hepatocellular carcinoma (HCC). To our knowledge, we report one of the few cases of drug-induced immune thrombocytopenia (D-ITP) in a hepatocellular carcinoma (HCC) patient receiving atezolizumab and bevacizumab.
Case Description/Methods: A 65-year-old male with Mavyret-treated HCV and alcoholic cirrhosis complicated by metastatic HCC, on active treatment with Atezolizumab/Bevacizumab, presented for hemoptysis and a bleeding lip ulcer. Vitals were stable and labs were significant for normal transaminases, INR, hemoglobin, and hemolysis labs. His ALP was 229 and platelets were 1. The patient was transfused 2 units of platelets with only transient improvement of platelets to 24, followed by an abrupt decrease to 1. On the peripheral smear, no platelets were visualized, and the abdominal US showed a right hepatic lobe malignant mass and splenomegaly. He was evaluated by hematology for ITP concerns and was started on IVIG and pulse dose dexamethasone. Bone marrow biopsy showed adequate megakaryopoiesis, no increase in blasts, or morphologic evidence of malignancy. The adequate megakaryocytes were suggestive of a peripheral destruction process. The patient had multiple transfusions during his stay with short-lived transient improvements. Despite therapy, he continued to be thrombocytopenic, pointing toward a diagnosis of D-ITP. The persistent thrombocytopenia was most likely due to the half-lives of atezolizumab (27 days) and bevacizumab (20 days), which would prolong the thrombocytopenia until washout. Eventually, the platelet count stabilized above 10k after a presumed washout, and the patient was discharged. Repeat platelet counts after discharge continued to be within normal range.
Discussion: ITP was suspected early on in the course of this patient's hospital stay. D-ITP was suspected after he did not respond to IVIG and steroids in the setting of recently receiving atezolizumab and bevacizumab. Monoclonal antibodies are becoming more prevalent in the treatment of cancers and thrombocytopenia is a rare side effect accounting for < 1% of patients¹. D-ITP should be on the differential diagnosis because removal of the offending monoclonal antibodies is required for washout, which should result in platelet count stabilization.
¹Shiuan E, et.al. Thrombocytopenia in patients with melanoma receiving immune checkpoint inhibitor therapy. 2017 Feb 21

Disclosures:
Avneet Singh, DO, Alexander Garcia, DO, Ishita Dhawan, MD, Tara Lautenslager, MD. P2568 - A Rare Case of Drug-Induced Immune Thrombocytopenia From Hepatocellular Carcinoma Treatment, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Cooper University Hospital, Camden, NJ
Introduction: Atezolizumab is an immune checkpoint inhibitor that binds PD-L1 and bevacizumab is an antiangiogenic that are considered a standard of care in patients with hepatocellular carcinoma (HCC). To our knowledge, we report one of the few cases of drug-induced immune thrombocytopenia (D-ITP) in a hepatocellular carcinoma (HCC) patient receiving atezolizumab and bevacizumab.
Case Description/Methods: A 65-year-old male with Mavyret-treated HCV and alcoholic cirrhosis complicated by metastatic HCC, on active treatment with Atezolizumab/Bevacizumab, presented for hemoptysis and a bleeding lip ulcer. Vitals were stable and labs were significant for normal transaminases, INR, hemoglobin, and hemolysis labs. His ALP was 229 and platelets were 1. The patient was transfused 2 units of platelets with only transient improvement of platelets to 24, followed by an abrupt decrease to 1. On the peripheral smear, no platelets were visualized, and the abdominal US showed a right hepatic lobe malignant mass and splenomegaly. He was evaluated by hematology for ITP concerns and was started on IVIG and pulse dose dexamethasone. Bone marrow biopsy showed adequate megakaryopoiesis, no increase in blasts, or morphologic evidence of malignancy. The adequate megakaryocytes were suggestive of a peripheral destruction process. The patient had multiple transfusions during his stay with short-lived transient improvements. Despite therapy, he continued to be thrombocytopenic, pointing toward a diagnosis of D-ITP. The persistent thrombocytopenia was most likely due to the half-lives of atezolizumab (27 days) and bevacizumab (20 days), which would prolong the thrombocytopenia until washout. Eventually, the platelet count stabilized above 10k after a presumed washout, and the patient was discharged. Repeat platelet counts after discharge continued to be within normal range.
Discussion: ITP was suspected early on in the course of this patient's hospital stay. D-ITP was suspected after he did not respond to IVIG and steroids in the setting of recently receiving atezolizumab and bevacizumab. Monoclonal antibodies are becoming more prevalent in the treatment of cancers and thrombocytopenia is a rare side effect accounting for < 1% of patients¹. D-ITP should be on the differential diagnosis because removal of the offending monoclonal antibodies is required for washout, which should result in platelet count stabilization.
¹Shiuan E, et.al. Thrombocytopenia in patients with melanoma receiving immune checkpoint inhibitor therapy. 2017 Feb 21

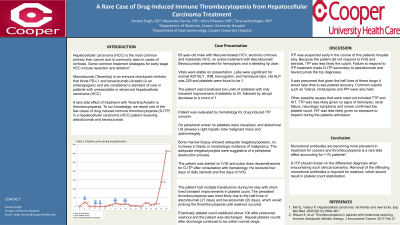
Figure: Title: Platelet count during the hospital stay
x-axis: Number of lab draw
y-axis: Platelet count
arrow: Platelet transfusion
x-axis: Number of lab draw
y-axis: Platelet count
arrow: Platelet transfusion
Disclosures:
Avneet Singh indicated no relevant financial relationships.
Alexander Garcia indicated no relevant financial relationships.
Ishita Dhawan indicated no relevant financial relationships.
Tara Lautenslager indicated no relevant financial relationships.
Avneet Singh, DO, Alexander Garcia, DO, Ishita Dhawan, MD, Tara Lautenslager, MD. P2568 - A Rare Case of Drug-Induced Immune Thrombocytopenia From Hepatocellular Carcinoma Treatment, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
