Monday Poster Session
Category: Liver
P2578 - Flood Syndrome: An Inundation of Complications
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Kelli Kosako Yost, MD
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Kelli Kosako Yost, MD, Xue Jing Li, MD, Natasha Narang, DO, Ma Ai Thanda Han, MD, Rohit Nathan, DO
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Up to 20% of patients with large-volume ascites will develop an umbilical hernia due to increased abdominal pressure and weakened musculature. Recurrent, uncontrolled ascites can lead to umbilical hernia rupture and extravasation of ascitic fluid, termed “Flood Syndrome”. Although rare, these patients are at risk of developing complications such as hypotension, incarceration of bowel, or peritonitis.
Case Description/Methods: The patient is a 68-year-old male with cirrhosis (secondary to alcohol use and treated Hepatitis C) complicated by ascites requiring large-volume paracentesis who presented after his umbilical hernia began spontaneously leaking ascitic fluid. The first hospital applied skin adhesive and sutures and discharged the patient. He then presented to a second hospital with stable vital signs and labs significant for sodium 130 mmol/L, INR 1.4, bilirubin 2.4 mg/dL, and creatinine 0.63 mg/dL (MELD 20). The patient was resuscitated with IV fluids, started on ciprofloxacin, and an ostomy bag was placed over the site. Surgery recommended medical management of ascites prior to any surgical intervention. He was then transferred to a tertiary care facility for TIPS (transjugular intrahepatic portosystemic shunting) evaluation. Herniorrhaphy with JP drain placement was completed, but TIPS was postponed due to persistent hyponatremia (115-122 mmol/L) and high MELD scores (25). The patient then developed leukocytosis (WBC 23.8 K/uL), acute kidney injury (creatinine 2.38 mg/dL), and hypotension. Blood cultures remained negative, but fluid taken from the JP drain grew scant enterococcus faecium with an ANC count of 1,907/mm3. Antibiotics were broadened to linezolid and piperacillin-tazobactam, and the patient was transferred to ICU for vasopressors. CT abdomen and pelvis demonstrated small to moderate pneumoperitoneum, which was likely secondary to recent surgery/drain placement. His condition continued to decline and he was placed on comfort care measures and died shortly after.
Discussion: Flood syndrome is a rare complication from recurrent, large-volume ascites. Stabilization of the patient with fluid resuscitation, electrolyte replacement, and prophylactic antibiotics are critical. Surgical closure and TIPS are commonly utilized, but surgery is often delayed due to the high risk of post-operative complications, specifically wound dehiscence and coagulopathy. Awareness of the high morbidity and mortality of this condition is paramount, and a multispecialty approach is necessary.

Disclosures:
Kelli Kosako Yost, MD, Xue Jing Li, MD, Natasha Narang, DO, Ma Ai Thanda Han, MD, Rohit Nathan, DO. P2578 - Flood Syndrome: An Inundation of Complications, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Arizona College of Medicine, Phoenix, AZ
Introduction: Up to 20% of patients with large-volume ascites will develop an umbilical hernia due to increased abdominal pressure and weakened musculature. Recurrent, uncontrolled ascites can lead to umbilical hernia rupture and extravasation of ascitic fluid, termed “Flood Syndrome”. Although rare, these patients are at risk of developing complications such as hypotension, incarceration of bowel, or peritonitis.
Case Description/Methods: The patient is a 68-year-old male with cirrhosis (secondary to alcohol use and treated Hepatitis C) complicated by ascites requiring large-volume paracentesis who presented after his umbilical hernia began spontaneously leaking ascitic fluid. The first hospital applied skin adhesive and sutures and discharged the patient. He then presented to a second hospital with stable vital signs and labs significant for sodium 130 mmol/L, INR 1.4, bilirubin 2.4 mg/dL, and creatinine 0.63 mg/dL (MELD 20). The patient was resuscitated with IV fluids, started on ciprofloxacin, and an ostomy bag was placed over the site. Surgery recommended medical management of ascites prior to any surgical intervention. He was then transferred to a tertiary care facility for TIPS (transjugular intrahepatic portosystemic shunting) evaluation. Herniorrhaphy with JP drain placement was completed, but TIPS was postponed due to persistent hyponatremia (115-122 mmol/L) and high MELD scores (25). The patient then developed leukocytosis (WBC 23.8 K/uL), acute kidney injury (creatinine 2.38 mg/dL), and hypotension. Blood cultures remained negative, but fluid taken from the JP drain grew scant enterococcus faecium with an ANC count of 1,907/mm3. Antibiotics were broadened to linezolid and piperacillin-tazobactam, and the patient was transferred to ICU for vasopressors. CT abdomen and pelvis demonstrated small to moderate pneumoperitoneum, which was likely secondary to recent surgery/drain placement. His condition continued to decline and he was placed on comfort care measures and died shortly after.
Discussion: Flood syndrome is a rare complication from recurrent, large-volume ascites. Stabilization of the patient with fluid resuscitation, electrolyte replacement, and prophylactic antibiotics are critical. Surgical closure and TIPS are commonly utilized, but surgery is often delayed due to the high risk of post-operative complications, specifically wound dehiscence and coagulopathy. Awareness of the high morbidity and mortality of this condition is paramount, and a multispecialty approach is necessary.

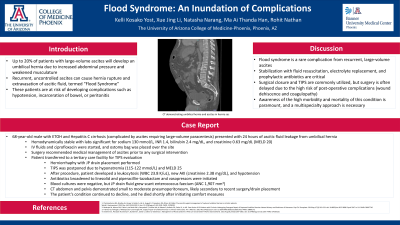
Figure: CT abdomen and pelvis without contrast demonstrating umbilical hernia
Disclosures:
Kelli Kosako Yost indicated no relevant financial relationships.
Xue Jing Li indicated no relevant financial relationships.
Natasha Narang indicated no relevant financial relationships.
Ma Ai Thanda Han indicated no relevant financial relationships.
Rohit Nathan indicated no relevant financial relationships.
Kelli Kosako Yost, MD, Xue Jing Li, MD, Natasha Narang, DO, Ma Ai Thanda Han, MD, Rohit Nathan, DO. P2578 - Flood Syndrome: An Inundation of Complications, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
