Monday Poster Session
Category: Liver
P2580 - An Investigation Beyond Alcohol Hepatitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Sarah Huang, MD
New York Presbyterian Brooklyn Methodist Hospital
Brooklyn, New York
Presenting Author(s)
Sarah Huang, MD1, Pratishtha Singh, MD1, Ezana Bekele, MD2, Ilan Weisberg, MD1
1New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist, Brooklyn, NY
Introduction: Autoimmune hepatitis (AIH) is an immune inflammatory liver disease that can be asymptomatic, and present as chronic disease or as acute liver failure. Its pathogenesis involves an immunological response toward hepatocyte autoantigens leading to progressive hepatic necroinflammation and fibrogenesis. Etiologies may be genetic predisposition linked to major histocompatibility complex loci, viral causes, or drugs (i.e. nitrofurantoin and minocycline).
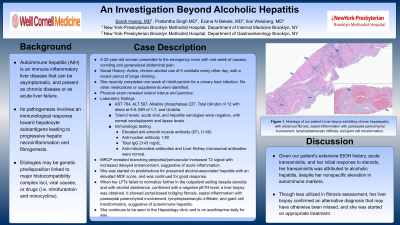
Case Description/Methods: A 32-year-old woman presented to the emergency room with one week of nausea, vomiting and generalized abdominal pain. She reported active, chronic alcohol use of 5 cocktails every other day, with a recent period of binge drinking. She recently completed one week of nitrofurantoin for a urinary tract infection. No other medications or supplements were identified. Physical exam revealed scleral icterus and jaundice. Laboratory results were remarkable for AST 764, ALT 507, alkaline phosphatase 227, total bilirubin of 12 with direct at 9.8, INR of 1.7, and urobilia. Tylenol levels, acute viral, and hepatitis serologies were negative, with normal ceruloplasmin and lipase levels. Immunologic testing revealed elevated anti-smooth muscle antibody (67), (1:40), anti-nuclear antibody 1:80, and total IgG 2143mg/dL. Anti-mitochondrial antibodies and liver kidney microsomal antibodies were normal. MRCP revealed branching periportal/perivascular increased T2 signal with increased delayed enhancement, suggestive of acute inflammation. She was started on prednisolone for presumed alcohol-associated hepatitis with an elevated MDF score, and was continued for good response. When her LFTs failed to normalize further in the outpatient setting despite steroids and with alcohol abstinence, confirmed with a negative pETH level, a liver biopsy was obtained. It showed portal-based bridging fibrosis, septal inflammation with paraseptal parenchymal involvement, lymphoplasmacytic infiltrate, and giant cell transformation, suggestive of autoimmune hepatitis. She continues to follow in the hepatology clinic and is on azathioprine daily for AIH.
Discussion: Given our patient’s extensive EtOH history, acute transaminitis, and her initial response to steroids, her transaminitis was attributed to alcoholic hepatitis, despite her nonspecific elevation in autoimmune markers. Though less utilized in fibrosis assessment, her liver biopsy confirmed an alternative diagnosis that may have otherwise been missed, and she was started on appropriate treatment.

Disclosures:
Sarah Huang, MD1, Pratishtha Singh, MD1, Ezana Bekele, MD2, Ilan Weisberg, MD1. P2580 - An Investigation Beyond Alcohol Hepatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist, Brooklyn, NY
Introduction: Autoimmune hepatitis (AIH) is an immune inflammatory liver disease that can be asymptomatic, and present as chronic disease or as acute liver failure. Its pathogenesis involves an immunological response toward hepatocyte autoantigens leading to progressive hepatic necroinflammation and fibrogenesis. Etiologies may be genetic predisposition linked to major histocompatibility complex loci, viral causes, or drugs (i.e. nitrofurantoin and minocycline).
Case Description/Methods: A 32-year-old woman presented to the emergency room with one week of nausea, vomiting and generalized abdominal pain. She reported active, chronic alcohol use of 5 cocktails every other day, with a recent period of binge drinking. She recently completed one week of nitrofurantoin for a urinary tract infection. No other medications or supplements were identified. Physical exam revealed scleral icterus and jaundice. Laboratory results were remarkable for AST 764, ALT 507, alkaline phosphatase 227, total bilirubin of 12 with direct at 9.8, INR of 1.7, and urobilia. Tylenol levels, acute viral, and hepatitis serologies were negative, with normal ceruloplasmin and lipase levels. Immunologic testing revealed elevated anti-smooth muscle antibody (67), (1:40), anti-nuclear antibody 1:80, and total IgG 2143mg/dL. Anti-mitochondrial antibodies and liver kidney microsomal antibodies were normal. MRCP revealed branching periportal/perivascular increased T2 signal with increased delayed enhancement, suggestive of acute inflammation. She was started on prednisolone for presumed alcohol-associated hepatitis with an elevated MDF score, and was continued for good response. When her LFTs failed to normalize further in the outpatient setting despite steroids and with alcohol abstinence, confirmed with a negative pETH level, a liver biopsy was obtained. It showed portal-based bridging fibrosis, septal inflammation with paraseptal parenchymal involvement, lymphoplasmacytic infiltrate, and giant cell transformation, suggestive of autoimmune hepatitis. She continues to follow in the hepatology clinic and is on azathioprine daily for AIH.
Discussion: Given our patient’s extensive EtOH history, acute transaminitis, and her initial response to steroids, her transaminitis was attributed to alcoholic hepatitis, despite her nonspecific elevation in autoimmune markers. Though less utilized in fibrosis assessment, her liver biopsy confirmed an alternative diagnosis that may have otherwise been missed, and she was started on appropriate treatment.

Figure: Histology of our patient’s liver biopsy exhibiting chronic hepatopathy with advanced fibrosis, septal inflammation with paraseptal parenchymal involvement, lymphoplasmacytic infiltrate, and giant cell transformation.
Disclosures:
Sarah Huang indicated no relevant financial relationships.
Pratishtha Singh indicated no relevant financial relationships.
Ezana Bekele indicated no relevant financial relationships.
Ilan Weisberg indicated no relevant financial relationships.
Sarah Huang, MD1, Pratishtha Singh, MD1, Ezana Bekele, MD2, Ilan Weisberg, MD1. P2580 - An Investigation Beyond Alcohol Hepatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
