Monday Poster Session
Category: Liver
P2596 - Spontaneous Adrenal Insufficiency in a Decompensated Cirrhotic Patient
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Kazi Haque, MD
UTH Health Science Center at Houston
Houston, TX
Presenting Author(s)
Kazi Haque, MD1, Andrew W. Zarker, BS1, Jennifer Ma, MD2, Stephen E. Glombicki, MD, MBA3, Jing Kees, MD4, Glynda Raynaldo, MD4, Elizabeth Lam, MD4
1UTH Health Science Center at Houston, Houston, TX; 2McGovern Medical School at UTHealth, Houston, TX; 3University of Texas Health Science Center, Houston, TX; 4Baylor College of Medicine, Houston, TX
Introduction: Decompensated cirrhosis can be challenging to manage and can vary in presentation. They require close monitoring due to increased mortality risks with SBP and bleeding. Here we have a case of spontaneous adrenal insufficiency (AI) in a clinically stable cirrhotic patient.
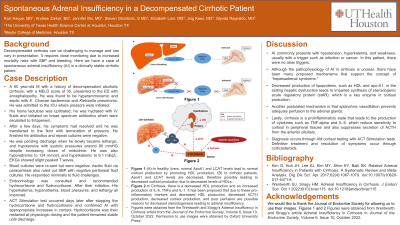
Case Description/Methods: A 60 year-old M with hx of decompensated alcoholic cirrhosis (MELD 35) presented with encephalopathy. He was found to be hyperammonemic and septic with E. Cloacae and Klebsiella pneumonia and admitted to ICU where pressors were initiated. His home lactulose was uptitrated; he was hydrated with IV fluids and initiated on broad spectrum antibiotics which escalated to Ertapenem. After a few days, his symptoms had resolved and was transferred to the floor with the removal of pressors. He finished his antibiotics and repeat cultures were negative. He was pending discharge when he slowly became lethargic, hypotensive despite midodrine, hyponatremic to 124, and hyperkalemic to 6.1. Cultures were re-sent but were negative. Ascitic fluid via therapeutic paracentesis also ruled out SBP. He responded minimally to fluids. Endocrine was consulted and recommended hydrocortisone and fludrocortisone. His hyperkalemia, hyponatremia, blood pressures, and lethargy all resolved. ACT Stimulation test occurred days later after stopping the hydrocortisone and fludrocortisone and confirmed AI. Hydrocortisone was then restarted and the patient remained stable until discharge.
Discussion: AI presents itself with hypotension, hyperkalemia, and weakness, but usually presents with a trigger such as infection or cancer. In this patient, there were no clear triggers. Although the pathophysiology of AI in cirrhosis is unclear, there have been many proposed mechanisms that support the concept of “hepatoadrenal syndrome.” Decreased production of lipoproteins, such as HDL and apo-A1, in the setting hepatic dysfunction leads to impaired synthesis of steroidogenic acute regulatory protein (stAR), which is a key enzyme in cortisol production. Another postulated mechanism is that splanchnic vasodilation prevents adequate perfusion to the adrenal glands. Lastly, cirrhosis is a proinflammatory state that leads to the production of cytokines such as TNF-alpha and IL-6, which reduce sensitivity to cortisol in peripheral tissues and also suppresses secretion of ACTH from the anterior pituitary. Diagnosis occurs through AM cortisol testing with ACT Stimulation tests. Definitive treatment and resolution of symptoms occur through corticosteroids.
Disclosures:
Kazi Haque, MD1, Andrew W. Zarker, BS1, Jennifer Ma, MD2, Stephen E. Glombicki, MD, MBA3, Jing Kees, MD4, Glynda Raynaldo, MD4, Elizabeth Lam, MD4. P2596 - Spontaneous Adrenal Insufficiency in a Decompensated Cirrhotic Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UTH Health Science Center at Houston, Houston, TX; 2McGovern Medical School at UTHealth, Houston, TX; 3University of Texas Health Science Center, Houston, TX; 4Baylor College of Medicine, Houston, TX
Introduction: Decompensated cirrhosis can be challenging to manage and can vary in presentation. They require close monitoring due to increased mortality risks with SBP and bleeding. Here we have a case of spontaneous adrenal insufficiency (AI) in a clinically stable cirrhotic patient.
Case Description/Methods: A 60 year-old M with hx of decompensated alcoholic cirrhosis (MELD 35) presented with encephalopathy. He was found to be hyperammonemic and septic with E. Cloacae and Klebsiella pneumonia and admitted to ICU where pressors were initiated. His home lactulose was uptitrated; he was hydrated with IV fluids and initiated on broad spectrum antibiotics which escalated to Ertapenem. After a few days, his symptoms had resolved and was transferred to the floor with the removal of pressors. He finished his antibiotics and repeat cultures were negative. He was pending discharge when he slowly became lethargic, hypotensive despite midodrine, hyponatremic to 124, and hyperkalemic to 6.1. Cultures were re-sent but were negative. Ascitic fluid via therapeutic paracentesis also ruled out SBP. He responded minimally to fluids. Endocrine was consulted and recommended hydrocortisone and fludrocortisone. His hyperkalemia, hyponatremia, blood pressures, and lethargy all resolved. ACT Stimulation test occurred days later after stopping the hydrocortisone and fludrocortisone and confirmed AI. Hydrocortisone was then restarted and the patient remained stable until discharge.
Discussion: AI presents itself with hypotension, hyperkalemia, and weakness, but usually presents with a trigger such as infection or cancer. In this patient, there were no clear triggers. Although the pathophysiology of AI in cirrhosis is unclear, there have been many proposed mechanisms that support the concept of “hepatoadrenal syndrome.” Decreased production of lipoproteins, such as HDL and apo-A1, in the setting hepatic dysfunction leads to impaired synthesis of steroidogenic acute regulatory protein (stAR), which is a key enzyme in cortisol production. Another postulated mechanism is that splanchnic vasodilation prevents adequate perfusion to the adrenal glands. Lastly, cirrhosis is a proinflammatory state that leads to the production of cytokines such as TNF-alpha and IL-6, which reduce sensitivity to cortisol in peripheral tissues and also suppresses secretion of ACTH from the anterior pituitary. Diagnosis occurs through AM cortisol testing with ACT Stimulation tests. Definitive treatment and resolution of symptoms occur through corticosteroids.
Disclosures:
Kazi Haque indicated no relevant financial relationships.
Andrew Zarker indicated no relevant financial relationships.
Jennifer Ma indicated no relevant financial relationships.
Stephen E. Glombicki indicated no relevant financial relationships.
Jing Kees indicated no relevant financial relationships.
Glynda Raynaldo indicated no relevant financial relationships.
Elizabeth Lam indicated no relevant financial relationships.
Kazi Haque, MD1, Andrew W. Zarker, BS1, Jennifer Ma, MD2, Stephen E. Glombicki, MD, MBA3, Jing Kees, MD4, Glynda Raynaldo, MD4, Elizabeth Lam, MD4. P2596 - Spontaneous Adrenal Insufficiency in a Decompensated Cirrhotic Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
