Monday Poster Session
Category: Liver
P2597 - A Rare Case of Campylobacter jejuni-Associated Hepatitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- HM
Hamsika Moparty, MD
Brooklyn Hospital Center
Brooklyn, New York
Presenting Author(s)
Hamsika Moparty, MD1, Enmanuel Then, 2, Saigopal R. Gujjula, 3, Praneeth Bandaru, MD1, Arnold Forlemu, MD, MPH1, Vikash Kumar, MD1, Sohrab Singh, MD1, Madhavi Reddy, MD1
1Brooklyn Hospital Center, Brooklyn, NY; 2Universidad Iberoamericana, Gazcue, Distrito Nacional, Dominican Republic; 3American University of Antigua, Coolidge, Saint John, Antigua and Barbuda
Introduction: Campylobacter species is a common culprit of bacterial diarrheal illnesses, affecting about 1.3 million patients yearly in the United States alone. Common manifestations include abdominal pain and bloody diarrhea, however certain extraintestinal manifestations can be life-threatening. We describe one such complication of campylobacter jejuni causing hepatitis in a young woman presenting with abdominal pain and diarrhea.
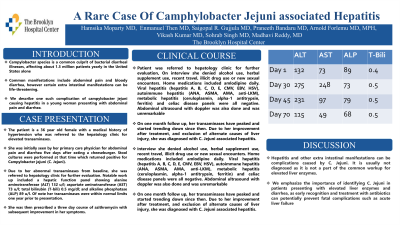
Case Description/Methods: The patient is a 36 year old female with a medical history of hypertension who was referred to the hepatology clinic for elevated transaminases. She was initially seen by her primary care physician for abdominal pain and diarrhea five days after eating a cheeseburger. Stool cultures were performed at that time which returned positive for Campylobacter jejuni (C. Jejuni). Other notable work up included a hepatic function panel showing alanine aminotransferase (ALT) 132 u/l; aspartate aminotransferase (AST) 73 u/l; total bilirubin (T-bili) 0.5 mg/dl; and alkaline phosphatase (ALP) 89 u/l. Of note her transaminases were within normal limits one year prior to presentation. She was then prescribed a three day course of azithromyzin with subsequent improvement in her symptoms. Due to her abnormal transaminases from baseline, she was referred to hepatology clinic for further evaluation. On interview she denied alcohol use, herbal supplement use, recent travel, illicit drug use or new sexual encounters. Home medications included amlodpine daily. Viral hepatitis (hepatitis A, B, C, D, E, CMV, EBV, HSV), autoimmune hepatitis (ANA, ASMA, AMA, anti-LKM), metabolic hepatitis (ceruloplasmin, alpha-1 antitrypsin, ferritin) and celiac disease panels were all negative. Abdominal ultrasound with doppler was also done and was unremarkable. On one month follow up, her transaminases have peaked and started trending down since then. Due to her improvement after treatment, and exclusion of alternate causes of liver injury, she was diagnosed with C.jejuni associated hepatitis.
Discussion: Hepatitis and other extra intestinal manifestations can be complications caused by C.jejuni. It is usually not diagnosed as it is not a part of the common workup for elevated liver enzymes. We emphasize the importance of identifying C. Jejuni in patients presenting with elevated liver enzymes and diarrhea, as early recognition and treatment with antibiotics can potentially prevent fatal complications such as acute liver failure.
Disclosures:
Hamsika Moparty, MD1, Enmanuel Then, 2, Saigopal R. Gujjula, 3, Praneeth Bandaru, MD1, Arnold Forlemu, MD, MPH1, Vikash Kumar, MD1, Sohrab Singh, MD1, Madhavi Reddy, MD1. P2597 - A Rare Case of Campylobacter jejuni-Associated Hepatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2Universidad Iberoamericana, Gazcue, Distrito Nacional, Dominican Republic; 3American University of Antigua, Coolidge, Saint John, Antigua and Barbuda
Introduction: Campylobacter species is a common culprit of bacterial diarrheal illnesses, affecting about 1.3 million patients yearly in the United States alone. Common manifestations include abdominal pain and bloody diarrhea, however certain extraintestinal manifestations can be life-threatening. We describe one such complication of campylobacter jejuni causing hepatitis in a young woman presenting with abdominal pain and diarrhea.
Case Description/Methods: The patient is a 36 year old female with a medical history of hypertension who was referred to the hepatology clinic for elevated transaminases. She was initially seen by her primary care physician for abdominal pain and diarrhea five days after eating a cheeseburger. Stool cultures were performed at that time which returned positive for Campylobacter jejuni (C. Jejuni). Other notable work up included a hepatic function panel showing alanine aminotransferase (ALT) 132 u/l; aspartate aminotransferase (AST) 73 u/l; total bilirubin (T-bili) 0.5 mg/dl; and alkaline phosphatase (ALP) 89 u/l. Of note her transaminases were within normal limits one year prior to presentation. She was then prescribed a three day course of azithromyzin with subsequent improvement in her symptoms. Due to her abnormal transaminases from baseline, she was referred to hepatology clinic for further evaluation. On interview she denied alcohol use, herbal supplement use, recent travel, illicit drug use or new sexual encounters. Home medications included amlodpine daily. Viral hepatitis (hepatitis A, B, C, D, E, CMV, EBV, HSV), autoimmune hepatitis (ANA, ASMA, AMA, anti-LKM), metabolic hepatitis (ceruloplasmin, alpha-1 antitrypsin, ferritin) and celiac disease panels were all negative. Abdominal ultrasound with doppler was also done and was unremarkable. On one month follow up, her transaminases have peaked and started trending down since then. Due to her improvement after treatment, and exclusion of alternate causes of liver injury, she was diagnosed with C.jejuni associated hepatitis.
Discussion: Hepatitis and other extra intestinal manifestations can be complications caused by C.jejuni. It is usually not diagnosed as it is not a part of the common workup for elevated liver enzymes. We emphasize the importance of identifying C. Jejuni in patients presenting with elevated liver enzymes and diarrhea, as early recognition and treatment with antibiotics can potentially prevent fatal complications such as acute liver failure.
Disclosures:
Hamsika Moparty indicated no relevant financial relationships.
Enmanuel Then indicated no relevant financial relationships.
Saigopal Gujjula indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Sohrab Singh indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Hamsika Moparty, MD1, Enmanuel Then, 2, Saigopal R. Gujjula, 3, Praneeth Bandaru, MD1, Arnold Forlemu, MD, MPH1, Vikash Kumar, MD1, Sohrab Singh, MD1, Madhavi Reddy, MD1. P2597 - A Rare Case of Campylobacter jejuni-Associated Hepatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
