Monday Poster Session
Category: Obesity
P2610 - Epidemiology and Implications of Concurrent Diagnosis of Eosinophilic Esophagitis and Obesity: A Comprehensive Global Population-Based Analysis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Mengdan Xie, MD
MetroHealth Medical Center
Cleveland, Ohio
Presenting Author(s)
Mengdan Xie, MD1, Lifu Deng, PhD2, Michael Kurin, MD3, Ronnie Fass, MD4, Gengqing Song, MD4
1MetroHealth Medical Center, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3MetroHealth, Cleveland, OH; 4MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Eosinophilic Esophagitis (EoE) is a chronic inflammatory condition characterized by immune-mediated eosinophils infiltration and esophageal remodeling. The incidence and prevalence of EoE and obesity have independently increased in the past decades, however there is sparse data about clinical implications of concurrent diagnosis of EoE and obesity.
Methods: The TriNetX electronic health records network, which involves 109 healthcare organizations in 14 countries, was utilized for this population-based study. The diagnosis of obesity was defined as patients with body mass index (BMI) of more than 30 kg/m2. Codes in all outpatient and inpatient encounters were used to identify patients with eosinophilic esophagitis (EoE) (ICD-10: K20.0). We estimated the incidence and prevalence of EoE in patients with obesity, and vice versa. The prevalence of hiatal hernia and GERD was compared in EoE patients with or without obesity. The prevalence of esophageal stricture, food impaction, and upper endoscopy (EGD) and endoscopic dilation, proton pump inhibitor (PPI) use, topical steroid use, were also analyzed as EoE-related clinical outcomes. We performed 1:1 propensity score matching for age, gender, ethnicity/race, alcohol use disorder, and tobacco use disorder.
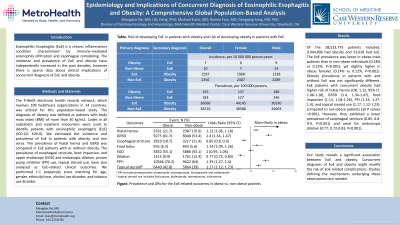
Results: Of the 28,523,773 patients included, 9,944,896 had obesity and 53,628 had EoE. The EoE prevalence was lower in obese male patients than in non-obese individuals (0.18% vs 0.25%, P< 0.001), yet slightly higher in obese females (0.14% vs 0.12%, P< 0.001). Obesity prevalence in patients with and without EoE was not significantly different. EoE patients with concurrent obesity had higher risk of hiatal hernia (OR: 1.12, 95% CI: 1.06-1.18), GERD (1.4, 1.34-1.47), food impaction (1.14, 1.04-1.26), PPI (1.33, 1.27-1.4), and topical steroid use (1.17, 1.12-1.23), compared to non-obese patients (all P values < 0.001). However, they exhibited a lower prevalence of esophageal stricture (0.85, 0.8-0.9, P< 0.001) and need for endoscopic dilation (0.77, 0.72-0.83, P< 0.001).
Discussion: Our study reveals a significant association between EoE and obesity. Concurrent diagnosis of EoE and obesity might modify the risk of EoE-related complications. Studies defining the mechanisms underlying these observations are needed.

Disclosures:
Mengdan Xie, MD1, Lifu Deng, PhD2, Michael Kurin, MD3, Ronnie Fass, MD4, Gengqing Song, MD4. P2610 - Epidemiology and Implications of Concurrent Diagnosis of Eosinophilic Esophagitis and Obesity: A Comprehensive Global Population-Based Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1MetroHealth Medical Center, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH; 3MetroHealth, Cleveland, OH; 4MetroHealth Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Eosinophilic Esophagitis (EoE) is a chronic inflammatory condition characterized by immune-mediated eosinophils infiltration and esophageal remodeling. The incidence and prevalence of EoE and obesity have independently increased in the past decades, however there is sparse data about clinical implications of concurrent diagnosis of EoE and obesity.
Methods: The TriNetX electronic health records network, which involves 109 healthcare organizations in 14 countries, was utilized for this population-based study. The diagnosis of obesity was defined as patients with body mass index (BMI) of more than 30 kg/m2. Codes in all outpatient and inpatient encounters were used to identify patients with eosinophilic esophagitis (EoE) (ICD-10: K20.0). We estimated the incidence and prevalence of EoE in patients with obesity, and vice versa. The prevalence of hiatal hernia and GERD was compared in EoE patients with or without obesity. The prevalence of esophageal stricture, food impaction, and upper endoscopy (EGD) and endoscopic dilation, proton pump inhibitor (PPI) use, topical steroid use, were also analyzed as EoE-related clinical outcomes. We performed 1:1 propensity score matching for age, gender, ethnicity/race, alcohol use disorder, and tobacco use disorder.
Results: Of the 28,523,773 patients included, 9,944,896 had obesity and 53,628 had EoE. The EoE prevalence was lower in obese male patients than in non-obese individuals (0.18% vs 0.25%, P< 0.001), yet slightly higher in obese females (0.14% vs 0.12%, P< 0.001). Obesity prevalence in patients with and without EoE was not significantly different. EoE patients with concurrent obesity had higher risk of hiatal hernia (OR: 1.12, 95% CI: 1.06-1.18), GERD (1.4, 1.34-1.47), food impaction (1.14, 1.04-1.26), PPI (1.33, 1.27-1.4), and topical steroid use (1.17, 1.12-1.23), compared to non-obese patients (all P values < 0.001). However, they exhibited a lower prevalence of esophageal stricture (0.85, 0.8-0.9, P< 0.001) and need for endoscopic dilation (0.77, 0.72-0.83, P< 0.001).
Discussion: Our study reveals a significant association between EoE and obesity. Concurrent diagnosis of EoE and obesity might modify the risk of EoE-related complications. Studies defining the mechanisms underlying these observations are needed.

Figure: Fig: Prevalence and ORs for the EoE-related outcomes in obese vs. non-obese patients
Disclosures:
Mengdan Xie indicated no relevant financial relationships.
Lifu Deng indicated no relevant financial relationships.
Michael Kurin indicated no relevant financial relationships.
Ronnie Fass indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Mengdan Xie, MD1, Lifu Deng, PhD2, Michael Kurin, MD3, Ronnie Fass, MD4, Gengqing Song, MD4. P2610 - Epidemiology and Implications of Concurrent Diagnosis of Eosinophilic Esophagitis and Obesity: A Comprehensive Global Population-Based Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
