Monday Poster Session
Category: Obesity
P2618 - Pancreatitis Associated with Gastric Balloons Insertion: A Systematic Review
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Ahmed I.A Swi, MD
University of Missouri-Columbia
Columbia, MO
Presenting Author(s)
Ahmed I.A. Swi, MD1, Muhammad Nadeem. Yousaf, MD2, Rizwan Ishtiaq, MD3, Sanket Basida, MD4, Mustafa Gandhi, MD1, Alexander Malik, MD5, Darian Fard, MD4, Faisal A.. Bukeirat, MD4, Pousette Hamid, MD, PhD6, Ghassan M. Hammoud, MD1
1University of Missouri-Columbia, Columbia, MO; 2University of Missouri, Columbia, MO; 3Academic Hospitalist, St. Francis Hospital, Hartford, CT; 4University of Missouri at Columbia, Columbia, MO; 5Summa Health System, Akron, OH; 6California Institute of Behavioral Neurosciences and Psychology, Fairfield, CA
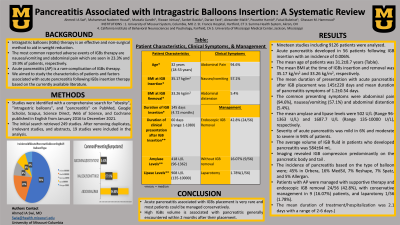
Introduction: Intragastric balloons (IGBs) therapy is an effective and non-surgical method for short-term weight loss. Acute pancreatitis (AP) is a rare complication of IGBs therapy. We aimed to investigate the clinical characteristics and factors associated with AP following IGBs insertion therapy based on the current literature.
Methods: Studies were identified with a comprehensive search for "obesity", "intragastric balloons", and "pancreatitis" on PubMed, Google Scholar, Scopus, Science Direct, Web of Science, and Cochrane published in English from January 2016 to December 2021. The initial search retrieved 249 studies. After removing duplicates, irrelevant studies, and abstracts 19 studies were included in the analysis. Descriptive analysis was performed using Stata/MP 17.
Results: Nineteen studies including 9126 patients were analyzed. Acute pancreatitis developed in 56 patients following IGB insertion with an incidence of 0.006%. The mean age of patients was 31.2±8.7 years. The mean BMI at the time of IGBs insertion and removal was 35.17 kg/m2 and 33.26 kg/m2 respectively. The mean duration of presentation with acute pancreatitis after IGB placement was 145±220 days and mean duration of pancreatitis symptoms of 1.2±0.54 days. The common presenting symptoms were abdominal pain (94.6%), nausea/vomiting (57.1%) and abdominal distention (5.4%). The mean amylase and lipase levels were 502 U/L (Range 96-1363 U/L) and 1687.7 U/L (Range 135-10000 U/L) respectively. Severity of acute pancreatitis was mild in 6% and moderate to severe in 94% of patients. The average volume of IGB fluid in patients who developed pancreatitis was 584±64 mL. Imaging revealed IGB compression predominantly on the pancreatic body and tail. The incidence of pancreatitis based on the type of balloon were; 45% in Orbera, followed by 16% MedSil, 7% Reshape, 7% Spatz, and 5% Allergan. Patients with AP were managed with supportive therapy and endoscopic IGB removal 24/56 (42.85%), laparotomy 1/56 (0.02%), and with conservative management in 9 (16.1%) patients. All patients were discharged after median hospitalization of 48 hours.
Discussion: Acute pancreatitis associated with IGBs placement is very rare and most patients could be managed conservatively. High IGBs volume is associated with pancreatitis generally encountered within 2 months after their placement.
Disclosures:
Ahmed I.A. Swi, MD1, Muhammad Nadeem. Yousaf, MD2, Rizwan Ishtiaq, MD3, Sanket Basida, MD4, Mustafa Gandhi, MD1, Alexander Malik, MD5, Darian Fard, MD4, Faisal A.. Bukeirat, MD4, Pousette Hamid, MD, PhD6, Ghassan M. Hammoud, MD1. P2618 - Pancreatitis Associated with Gastric Balloons Insertion: A Systematic Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Missouri-Columbia, Columbia, MO; 2University of Missouri, Columbia, MO; 3Academic Hospitalist, St. Francis Hospital, Hartford, CT; 4University of Missouri at Columbia, Columbia, MO; 5Summa Health System, Akron, OH; 6California Institute of Behavioral Neurosciences and Psychology, Fairfield, CA
Introduction: Intragastric balloons (IGBs) therapy is an effective and non-surgical method for short-term weight loss. Acute pancreatitis (AP) is a rare complication of IGBs therapy. We aimed to investigate the clinical characteristics and factors associated with AP following IGBs insertion therapy based on the current literature.
Methods: Studies were identified with a comprehensive search for "obesity", "intragastric balloons", and "pancreatitis" on PubMed, Google Scholar, Scopus, Science Direct, Web of Science, and Cochrane published in English from January 2016 to December 2021. The initial search retrieved 249 studies. After removing duplicates, irrelevant studies, and abstracts 19 studies were included in the analysis. Descriptive analysis was performed using Stata/MP 17.
Results: Nineteen studies including 9126 patients were analyzed. Acute pancreatitis developed in 56 patients following IGB insertion with an incidence of 0.006%. The mean age of patients was 31.2±8.7 years. The mean BMI at the time of IGBs insertion and removal was 35.17 kg/m2 and 33.26 kg/m2 respectively. The mean duration of presentation with acute pancreatitis after IGB placement was 145±220 days and mean duration of pancreatitis symptoms of 1.2±0.54 days. The common presenting symptoms were abdominal pain (94.6%), nausea/vomiting (57.1%) and abdominal distention (5.4%). The mean amylase and lipase levels were 502 U/L (Range 96-1363 U/L) and 1687.7 U/L (Range 135-10000 U/L) respectively. Severity of acute pancreatitis was mild in 6% and moderate to severe in 94% of patients. The average volume of IGB fluid in patients who developed pancreatitis was 584±64 mL. Imaging revealed IGB compression predominantly on the pancreatic body and tail. The incidence of pancreatitis based on the type of balloon were; 45% in Orbera, followed by 16% MedSil, 7% Reshape, 7% Spatz, and 5% Allergan. Patients with AP were managed with supportive therapy and endoscopic IGB removal 24/56 (42.85%), laparotomy 1/56 (0.02%), and with conservative management in 9 (16.1%) patients. All patients were discharged after median hospitalization of 48 hours.
Discussion: Acute pancreatitis associated with IGBs placement is very rare and most patients could be managed conservatively. High IGBs volume is associated with pancreatitis generally encountered within 2 months after their placement.
Disclosures:
Ahmed Swi indicated no relevant financial relationships.
Muhammad Yousaf indicated no relevant financial relationships.
Rizwan Ishtiaq indicated no relevant financial relationships.
Sanket Basida indicated no relevant financial relationships.
Mustafa Gandhi indicated no relevant financial relationships.
Alexander Malik indicated no relevant financial relationships.
Darian Fard indicated no relevant financial relationships.
Faisal Bukeirat indicated no relevant financial relationships.
Pousette Hamid indicated no relevant financial relationships.
Ghassan Hammoud indicated no relevant financial relationships.
Ahmed I.A. Swi, MD1, Muhammad Nadeem. Yousaf, MD2, Rizwan Ishtiaq, MD3, Sanket Basida, MD4, Mustafa Gandhi, MD1, Alexander Malik, MD5, Darian Fard, MD4, Faisal A.. Bukeirat, MD4, Pousette Hamid, MD, PhD6, Ghassan M. Hammoud, MD1. P2618 - Pancreatitis Associated with Gastric Balloons Insertion: A Systematic Review, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
