Monday Poster Session
Category: Small Intestine
P2632 - Association of Celiac Disease and Atrial Fibrillation: A National Inpatient Database Study
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Rutwik Pradeep Sharma, MD
Rochester Regional Health / Unity Hospital
Rochester, NY
Presenting Author(s)
Rutwik Pradeep Sharma, MD1, Ali Jaan, MD2, Ahmed Shehadah, MD2, Ese Uwagbale, MD2, Alexander Kusnik, MD3, Mythili Menon Pathiyil, MD4, Ari Chodos, MD5
1Rochester Regional Health / Unity Hospital, Rochester, NY; 2Rochester General Hospital, Rochester, NY; 3Rochester Regional Health, Rochester, NM; 4Saint Vincent Hospital, Worcester, MA; 5Unity Hospital, Rochester, NY
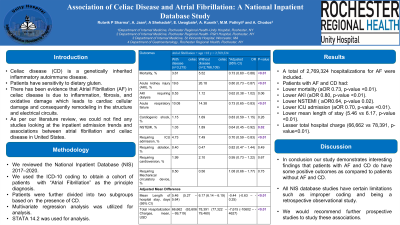
Introduction: Celiac disease (CD) is an inherited autoimmune disease. Patients have sensitivity to dietary gluten, which leads to lymphocytic infiltration, inflammation, and villous atrophy in the small intestine. Atrial fibrillation (AF) is one of the diseases, which is associated with celiac disease. There has been evidence that AF in CD is due to inflammation, fibrosis, and oxidative damage which leads to cardiac cellular damage and consequently remodeling in the structure and electrical circuits. As per our literature review, we could not find any studies looking at the inpatient admission trends and associations between AF and CD in the USA. We tried to address this with our study.
Methods: We retrospectively reviewed the National Inpatient Database (NIS) 2017 – 2020. We used International Classification of Diseases, Tenth Revision, Clinical Modifications (ICD-10- CM) codes to include adult patients (aged ≥18 years) hospitalized with the principal diagnosis of “Atrial fibrillation”. Patients were further divided into two subgroups based on the presence of CD. This database does not disclose patient identifications; hence, institutional review board approval is not required. Multivariate regression analysis was utilized to compare AF outcomes in patients with and without CD. STATA 14.2 was used for analysis.
Results: 2,769,324 hospitalizations for AF were included. AF patients with underlying CD were mostly White and there was female predominance (63.45% vs 46.64%, P< 0.01) as compared to those without CD. After adjusting common confounding variables (including conditions known to trigger AF), outcomes were evaluated. Patients with AF and CD had lower mortality (aOR 0.73, p-value < 0.01), lower AKI (aOR 0.80, p-value < 0.01), lower NSTEMI (aOR 0.64, p-value 0.02), lower ICU admission (aOR 0.70, p-value < 0.01), lower mean length of stay (5.46 vs 6.17, p-value < 0.01) and lesser total hospital charge (66,662 vs 78,391, p-value< 0.01) as compared to patients with AF without CD.
Discussion: Our study demonstrates interesting association findings in patients with atrial fibrillation and celiac disease to those with atrial fibrillation without celiac disease:
All NIS database studies have certain limitations such as improper coding and being a retrospective observational study. We would recommend further prospective studies to study these associations.
Disclosures:
Rutwik Pradeep Sharma, MD1, Ali Jaan, MD2, Ahmed Shehadah, MD2, Ese Uwagbale, MD2, Alexander Kusnik, MD3, Mythili Menon Pathiyil, MD4, Ari Chodos, MD5. P2632 - Association of Celiac Disease and Atrial Fibrillation: A National Inpatient Database Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rochester Regional Health / Unity Hospital, Rochester, NY; 2Rochester General Hospital, Rochester, NY; 3Rochester Regional Health, Rochester, NM; 4Saint Vincent Hospital, Worcester, MA; 5Unity Hospital, Rochester, NY
Introduction: Celiac disease (CD) is an inherited autoimmune disease. Patients have sensitivity to dietary gluten, which leads to lymphocytic infiltration, inflammation, and villous atrophy in the small intestine. Atrial fibrillation (AF) is one of the diseases, which is associated with celiac disease. There has been evidence that AF in CD is due to inflammation, fibrosis, and oxidative damage which leads to cardiac cellular damage and consequently remodeling in the structure and electrical circuits. As per our literature review, we could not find any studies looking at the inpatient admission trends and associations between AF and CD in the USA. We tried to address this with our study.
Methods: We retrospectively reviewed the National Inpatient Database (NIS) 2017 – 2020. We used International Classification of Diseases, Tenth Revision, Clinical Modifications (ICD-10- CM) codes to include adult patients (aged ≥18 years) hospitalized with the principal diagnosis of “Atrial fibrillation”. Patients were further divided into two subgroups based on the presence of CD. This database does not disclose patient identifications; hence, institutional review board approval is not required. Multivariate regression analysis was utilized to compare AF outcomes in patients with and without CD. STATA 14.2 was used for analysis.
Results: 2,769,324 hospitalizations for AF were included. AF patients with underlying CD were mostly White and there was female predominance (63.45% vs 46.64%, P< 0.01) as compared to those without CD. After adjusting common confounding variables (including conditions known to trigger AF), outcomes were evaluated. Patients with AF and CD had lower mortality (aOR 0.73, p-value < 0.01), lower AKI (aOR 0.80, p-value < 0.01), lower NSTEMI (aOR 0.64, p-value 0.02), lower ICU admission (aOR 0.70, p-value < 0.01), lower mean length of stay (5.46 vs 6.17, p-value < 0.01) and lesser total hospital charge (66,662 vs 78,391, p-value< 0.01) as compared to patients with AF without CD.
Discussion: Our study demonstrates interesting association findings in patients with atrial fibrillation and celiac disease to those with atrial fibrillation without celiac disease:
- Lower mortality rate
- Lower AKI rate
- Lower NSTEMI rate
- Lower ICU admission rate
- Lower mean length of stay in the hospital
- Lower total hospital charges
All NIS database studies have certain limitations such as improper coding and being a retrospective observational study. We would recommend further prospective studies to study these associations.
Disclosures:
Rutwik Pradeep Sharma indicated no relevant financial relationships.
Ali Jaan indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Ese Uwagbale indicated no relevant financial relationships.
Alexander Kusnik indicated no relevant financial relationships.
Mythili Menon Pathiyil indicated no relevant financial relationships.
Ari Chodos indicated no relevant financial relationships.
Rutwik Pradeep Sharma, MD1, Ali Jaan, MD2, Ahmed Shehadah, MD2, Ese Uwagbale, MD2, Alexander Kusnik, MD3, Mythili Menon Pathiyil, MD4, Ari Chodos, MD5. P2632 - Association of Celiac Disease and Atrial Fibrillation: A National Inpatient Database Study, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
