Monday Poster Session
Category: Small Intestine
P2646 - Pancreatic Elastase Deficiency in Gastrointestinal Strongyloidiasis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- VM
Valeria Martinez Lebron, MD
George Washington University Hospital
Washington, DC
Presenting Author(s)
Valeria Martinez Lebron, MD1, Junseo B. Lee, MD2, Samuel A. Schueler, MD1, Marie L. Borum, MD, EdD, MPH3, Thomas Huebner, MD4, Natasha Kamal, MD4
1George Washington University Hospital, Washington, DC; 2George Washington University School of Medicine and Health Sciences, Washington, DC; 3George Washington University Medical Center, Washington, DC; 4Frederick Gastroenterology Associates, Frederick, MD
Introduction: Strongyloides stercoralis can cause infection often involving the intestines, skin, and lung. We presented a patient with strongyloidiasis who exhibited extraintestinal manifestations, including pancreatic exocrine insufficiency (PEI).
Case Description/Methods:
A 47-year-old man with hypertension presented with fatigue, shortness of breath, cough, and chest pressure. He previously took oral steroids for 12 days for suspected asthma exacerbation. PFT, CT chest, and cardiac evaluation were normal. QuantiFERON-TB test was positive, but bronchoalveolar lavage was negative. Laboratory evaluation showed peripheral eosinophilia. The patient tried bronchodilators and eosinophilic inhibitors with no improvement. He later developed abdominal pain in the left lower and right upper quadrants with diarrhea, hemoptysis, epistaxis, and unintentional weight loss of 45 pounds over one month. Breath testing showed increased methane. Fecal pancreatic elastase was less than 50. He was treated with neomycin, rifaximin, and creon. Lipase, ANA, AMA, ASMA, IgG4, and inflammatory markers were normal. Tests for celiac disease, HIV, and Sjogren’s were negative.
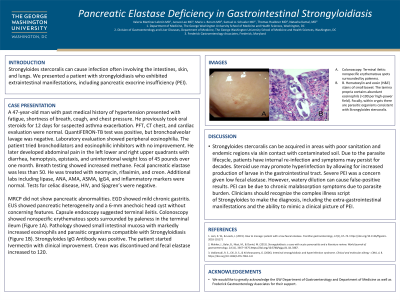
MRCP did not show pancreatic abnormalities. EGD showed mild chronic gastritis. EUS showed pancreatic heterogeneity and a 6-mm anechoic head cyst without concerning features. Capsule endoscopy suggested terminal ileitis. Colonoscopy showed nonspecific erythematous spots surrounded by paleness in the terminal ileum (Figure 1A). Pathology showed small intestinal mucosa with markedly increased eosinophils and parasitic organisms compatible with Strongyloidiasis (Figure 1B). Strongyloides IgG Antibody was positive. The patient started Ivermectin with clinical improvement. Creon was discontinued and fecal elastase increased to 120.
Discussion: Strongyloides stercoralis can be acquired in areas with poor sanitation and endemic regions via skin contact with contaminated soil. Due to the parasite lifecycle, patients have internal re-infection and symptoms may persist for decades. Steroid use may promote hyperinfection by allowing for increased production of larvae in the gastrointestinal tract. Severe PEI was a concern given low fecal elastase. However, watery dilution can cause false-positive results. PEI can be due to chronic malabsorption symptoms due to parasite burden. Clinicians should recognize the complex illness script of Strongyloides to make the diagnosis, including the extra-gastrointestinal manifestations and the ability to mimic a clinical picture of PEI.

Disclosures:
Valeria Martinez Lebron, MD1, Junseo B. Lee, MD2, Samuel A. Schueler, MD1, Marie L. Borum, MD, EdD, MPH3, Thomas Huebner, MD4, Natasha Kamal, MD4. P2646 - Pancreatic Elastase Deficiency in Gastrointestinal Strongyloidiasis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1George Washington University Hospital, Washington, DC; 2George Washington University School of Medicine and Health Sciences, Washington, DC; 3George Washington University Medical Center, Washington, DC; 4Frederick Gastroenterology Associates, Frederick, MD
Introduction: Strongyloides stercoralis can cause infection often involving the intestines, skin, and lung. We presented a patient with strongyloidiasis who exhibited extraintestinal manifestations, including pancreatic exocrine insufficiency (PEI).
Case Description/Methods:
A 47-year-old man with hypertension presented with fatigue, shortness of breath, cough, and chest pressure. He previously took oral steroids for 12 days for suspected asthma exacerbation. PFT, CT chest, and cardiac evaluation were normal. QuantiFERON-TB test was positive, but bronchoalveolar lavage was negative. Laboratory evaluation showed peripheral eosinophilia. The patient tried bronchodilators and eosinophilic inhibitors with no improvement. He later developed abdominal pain in the left lower and right upper quadrants with diarrhea, hemoptysis, epistaxis, and unintentional weight loss of 45 pounds over one month. Breath testing showed increased methane. Fecal pancreatic elastase was less than 50. He was treated with neomycin, rifaximin, and creon. Lipase, ANA, AMA, ASMA, IgG4, and inflammatory markers were normal. Tests for celiac disease, HIV, and Sjogren’s were negative.
MRCP did not show pancreatic abnormalities. EGD showed mild chronic gastritis. EUS showed pancreatic heterogeneity and a 6-mm anechoic head cyst without concerning features. Capsule endoscopy suggested terminal ileitis. Colonoscopy showed nonspecific erythematous spots surrounded by paleness in the terminal ileum (Figure 1A). Pathology showed small intestinal mucosa with markedly increased eosinophils and parasitic organisms compatible with Strongyloidiasis (Figure 1B). Strongyloides IgG Antibody was positive. The patient started Ivermectin with clinical improvement. Creon was discontinued and fecal elastase increased to 120.
Discussion: Strongyloides stercoralis can be acquired in areas with poor sanitation and endemic regions via skin contact with contaminated soil. Due to the parasite lifecycle, patients have internal re-infection and symptoms may persist for decades. Steroid use may promote hyperinfection by allowing for increased production of larvae in the gastrointestinal tract. Severe PEI was a concern given low fecal elastase. However, watery dilution can cause false-positive results. PEI can be due to chronic malabsorption symptoms due to parasite burden. Clinicians should recognize the complex illness script of Strongyloides to make the diagnosis, including the extra-gastrointestinal manifestations and the ability to mimic a clinical picture of PEI.

Figure: 1A. Colonoscopy: Terminal ileitis: nonspecific erythematous spots surrounded by paleness. 1B. Hematoxylin and eosin (H&E) stains of small bowel. The lamina propria contains abundant eosinophils (>100 per high-power field). Focally, within crypts there are parasitic organisms consistent with Strongyloides stercoralis.
Disclosures:
Valeria Martinez Lebron indicated no relevant financial relationships.
Junseo Lee indicated no relevant financial relationships.
Samuel Schueler indicated no relevant financial relationships.
Marie Borum: Takeda – Advisory Committee/Board Member, Speakers Bureau.
Thomas Huebner indicated no relevant financial relationships.
Natasha Kamal: Bristol Myers Squibb – Speakers Bureau.
Valeria Martinez Lebron, MD1, Junseo B. Lee, MD2, Samuel A. Schueler, MD1, Marie L. Borum, MD, EdD, MPH3, Thomas Huebner, MD4, Natasha Kamal, MD4. P2646 - Pancreatic Elastase Deficiency in Gastrointestinal Strongyloidiasis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
