Monday Poster Session
Category: Small Intestine
P2652 - Unveiling the Catastrophic Bowel Ischemia: A Challenging Case of Intestinal Ischemia in Systemic Lupus Erythematosus
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Abdellatif Ismail, MBBS, MD
University of Maryland Medical Center Midtown Campus
Baltimore, MD
Presenting Author(s)
Abdellatif Ismail, MBBS, MD1, Duha Zaffar, MBBS, MD2, Ahmad Khalaf, MD3, Mohammed Rifat Shaik, MBBS1, Jamal Mikdashi, MD4, Raymond Kim, MD, DM4
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2University of Maryland Medical Center Midtown Campus, Baltimore, MD; 3Hennepin Healthcare, Minneapolis, MN; 4University of Maryland Medical Center, Baltimore, MD
Introduction: Vascular manifestations of systemic lupus erythematosus (SLE) include vasculitis and thrombosis. Here we present a case of SLE complicated by catastrophic intestinal ischemia.
Case Description/Methods: A 36-year-old woman with SLE since age 25 had at baseline Raynaud's phenomenon, dermal vasculitis, and lupus nephritis.
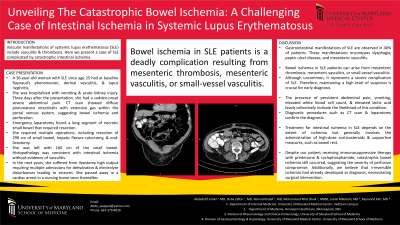
She was admitted to our hospital with acute kidney injury and developed sudden-onset severe abdominal pain three days after her presentation. Abdomen CT scan showed diffuse pneumatosis intestinalis with extensive gas within the portal venous system, suggesting bowel ischemia and perforation.
An emergency laparotomy revealed a long segment of necrotic small bowel that required resection. Over the following weeks, she required multiple operations, including resection of 290 cm of the small bowel, a hepatic flexure colectomy, end-ileostomy, and Hartman pouch creation. She was left with 160 cm of the small bowel. Histopathology was consistent with intestinal ischemia without evidence of vasculitis. Septic shock and acute respiratory distress syndrome further complicated the hospital course. In the next two years, she resided in a nursing home and suffered from ileostomy high output requiring multiple admissions for dehydration and electrolyte disturbances, including an admission with seizures due to severe hypocalcemia. She eventually passed away in a cardiac arrest.
Discussion: Gastrointestinal manifestations of SLE are observed in 40% of patients. These manifestations encompass dysphagia, peptic ulcer disease, and mesenteric vasculitis. Bowel ischemia in SLE patients can arise from mesenteric thrombosis, mesenteric vasculitis, or small-vessel vasculitis. Although uncommon, it represents a severe complication of SLE, and maintaining a high level of suspicion is crucial for early diagnosis. The presence of persistent abdominal pain, vomiting, elevated white blood cell count, and lactic acid levels collectively indicate the likelihood of this condition. Diagnostic modalities such as CT scan and laparotomy confirm the diagnosis. Treatment for intestinal ischemia in SLE generally involves the administration of high-dose corticosteroids and supportive measures, including bowel rest. Despite our patient receiving immunosuppressive therapy with prednisone and cyclophosphamide, catastrophic bowel ischemia still occurred, suggesting severe perfusion compromise. Additionally, we believe irreversible ischemia and necrosis had already developed at diagnosis, necessitating surgical intervention.

Disclosures:
Abdellatif Ismail, MBBS, MD1, Duha Zaffar, MBBS, MD2, Ahmad Khalaf, MD3, Mohammed Rifat Shaik, MBBS1, Jamal Mikdashi, MD4, Raymond Kim, MD, DM4. P2652 - Unveiling the Catastrophic Bowel Ischemia: A Challenging Case of Intestinal Ischemia in Systemic Lupus Erythematosus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2University of Maryland Medical Center Midtown Campus, Baltimore, MD; 3Hennepin Healthcare, Minneapolis, MN; 4University of Maryland Medical Center, Baltimore, MD
Introduction: Vascular manifestations of systemic lupus erythematosus (SLE) include vasculitis and thrombosis. Here we present a case of SLE complicated by catastrophic intestinal ischemia.
Case Description/Methods: A 36-year-old woman with SLE since age 25 had at baseline Raynaud's phenomenon, dermal vasculitis, and lupus nephritis.
She was admitted to our hospital with acute kidney injury and developed sudden-onset severe abdominal pain three days after her presentation. Abdomen CT scan showed diffuse pneumatosis intestinalis with extensive gas within the portal venous system, suggesting bowel ischemia and perforation.
An emergency laparotomy revealed a long segment of necrotic small bowel that required resection. Over the following weeks, she required multiple operations, including resection of 290 cm of the small bowel, a hepatic flexure colectomy, end-ileostomy, and Hartman pouch creation. She was left with 160 cm of the small bowel. Histopathology was consistent with intestinal ischemia without evidence of vasculitis. Septic shock and acute respiratory distress syndrome further complicated the hospital course. In the next two years, she resided in a nursing home and suffered from ileostomy high output requiring multiple admissions for dehydration and electrolyte disturbances, including an admission with seizures due to severe hypocalcemia. She eventually passed away in a cardiac arrest.
Discussion: Gastrointestinal manifestations of SLE are observed in 40% of patients. These manifestations encompass dysphagia, peptic ulcer disease, and mesenteric vasculitis. Bowel ischemia in SLE patients can arise from mesenteric thrombosis, mesenteric vasculitis, or small-vessel vasculitis. Although uncommon, it represents a severe complication of SLE, and maintaining a high level of suspicion is crucial for early diagnosis. The presence of persistent abdominal pain, vomiting, elevated white blood cell count, and lactic acid levels collectively indicate the likelihood of this condition. Diagnostic modalities such as CT scan and laparotomy confirm the diagnosis. Treatment for intestinal ischemia in SLE generally involves the administration of high-dose corticosteroids and supportive measures, including bowel rest. Despite our patient receiving immunosuppressive therapy with prednisone and cyclophosphamide, catastrophic bowel ischemia still occurred, suggesting severe perfusion compromise. Additionally, we believe irreversible ischemia and necrosis had already developed at diagnosis, necessitating surgical intervention.

Figure: Abdomen CT scan showing intramural and intraperitoneal gas suggesting intestinal perforation.
Case courtesy of Mohammadtaghi Niknejad, Radiopaedia.org, rID: 152391
Case courtesy of Mohammadtaghi Niknejad, Radiopaedia.org, rID: 152391
Disclosures:
Abdellatif Ismail indicated no relevant financial relationships.
Duha Zaffar indicated no relevant financial relationships.
Ahmad Khalaf indicated no relevant financial relationships.
Mohammed Rifat Shaik indicated no relevant financial relationships.
Jamal Mikdashi indicated no relevant financial relationships.
Raymond Kim: Apollo Endosurgery – Consultant. Cook medical – Consultant.
Abdellatif Ismail, MBBS, MD1, Duha Zaffar, MBBS, MD2, Ahmad Khalaf, MD3, Mohammed Rifat Shaik, MBBS1, Jamal Mikdashi, MD4, Raymond Kim, MD, DM4. P2652 - Unveiling the Catastrophic Bowel Ischemia: A Challenging Case of Intestinal Ischemia in Systemic Lupus Erythematosus, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
