Monday Poster Session
Category: Small Intestine
P2661 - Periampullary Duodenal Diverticulitis - Another Cause for Acute Pancreatitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- AK
Ayesha Khan, DO
University of Texas Medical Branch
Galveston, TX
Presenting Author(s)
Ayesha Khan, DO1, Kian Abdul-Baki, DO1, Keegan Colletier, MD2, Douglas Tyler, MD1, Alexander Perez, MD3, Maryamnaz Falamaki, MD4, Sreeram Parupudi, MD1
1University of Texas Medical Branch, Galveston, TX; 2UTMB Galveston, Texas City, TX; 3UTMB, Galveston, TX; 4UTMB-Galveston, Galveston, TX
Introduction: Small bowel diverticula are uncommon and usually asymptomatic. Although rare, complications include abdominal pain, small bowel diverticulitis, small bowel perforation, pancreaticobiliary obstruction, and related sequelae (i.e., ascending cholangitis, pancreatitis). We present a case of peri-ampullary duodenal diverticulitis successfully managed conservatively.
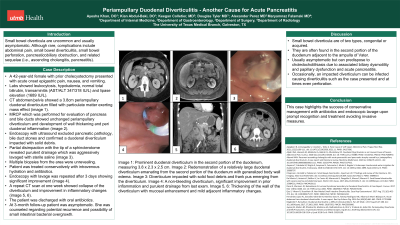
Case Description/Methods: A 42-year-old female with prior cholecystectomy presented with acute onset epigastric pain, nausea, and vomiting. Labs showed leukocytosis, hypokalemia, normal total bilirubin, transaminitis (AST/ALT 347/318 IU/L) and lipase elevation (1689 IU/L). CT abdomen/pelvis showed a 3.8cm periampullary duodenal diverticulum filled with particulate matter exerting mass effect (image 1). MRCP which performed for evaluation of pancreas and bile ducts showed unchanged periampullary diverticulum and development of wall thickening and peri duodenal inflammation (image 2). Endoscopy with ultrasound excluded pancreatic pathology, bile duct stones and confirmed a duodenal diverticulum impacted with solid debris. Partial disimpaction with the tip of a sphincterotome revealed purulent drainage which was aggressively lavaged with sterile saline (image 3). Multiple biopsies from the area were unrevealing. She was treated conservatively as a case of acute periampullary duodenal diverticulitis with mild pancreatitis by intravenous hydration and antibiotics. Endoscopy with lavage was repeated after 3 days showing significant improvement (image 4). A repeat CT scan at one week showed collapse of the diverticulum and improvement in inflammatory changes (image 5, 6). The patient was discharged with oral antibiotics. At 3month follow-up she was totally asymptomatic with normal liver enzymes. She was counseled regarding potential recurrence and possibility of small intestinal bacterial overgrowth.
Discussion: Small bowel diverticula are of two types, congenital or acquired. They are often found in the second portion of the duodenum adjacent to the ampulla of Vater and are usually asymptomatic but can predispose to choledocholithiasis due to associated biliary dysmotility and papillary dysfunction. Occasionally, an impacted diverticulum can be infected causing diverticulitis such as the case presented and at times even perforation. This case highlights the success of conservative management with antibiotics and endoscopic lavage upon prompt recognition and treatment avoiding invasive measures.

Disclosures:
Ayesha Khan, DO1, Kian Abdul-Baki, DO1, Keegan Colletier, MD2, Douglas Tyler, MD1, Alexander Perez, MD3, Maryamnaz Falamaki, MD4, Sreeram Parupudi, MD1. P2661 - Periampullary Duodenal Diverticulitis - Another Cause for Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Medical Branch, Galveston, TX; 2UTMB Galveston, Texas City, TX; 3UTMB, Galveston, TX; 4UTMB-Galveston, Galveston, TX
Introduction: Small bowel diverticula are uncommon and usually asymptomatic. Although rare, complications include abdominal pain, small bowel diverticulitis, small bowel perforation, pancreaticobiliary obstruction, and related sequelae (i.e., ascending cholangitis, pancreatitis). We present a case of peri-ampullary duodenal diverticulitis successfully managed conservatively.
Case Description/Methods: A 42-year-old female with prior cholecystectomy presented with acute onset epigastric pain, nausea, and vomiting. Labs showed leukocytosis, hypokalemia, normal total bilirubin, transaminitis (AST/ALT 347/318 IU/L) and lipase elevation (1689 IU/L). CT abdomen/pelvis showed a 3.8cm periampullary duodenal diverticulum filled with particulate matter exerting mass effect (image 1). MRCP which performed for evaluation of pancreas and bile ducts showed unchanged periampullary diverticulum and development of wall thickening and peri duodenal inflammation (image 2). Endoscopy with ultrasound excluded pancreatic pathology, bile duct stones and confirmed a duodenal diverticulum impacted with solid debris. Partial disimpaction with the tip of a sphincterotome revealed purulent drainage which was aggressively lavaged with sterile saline (image 3). Multiple biopsies from the area were unrevealing. She was treated conservatively as a case of acute periampullary duodenal diverticulitis with mild pancreatitis by intravenous hydration and antibiotics. Endoscopy with lavage was repeated after 3 days showing significant improvement (image 4). A repeat CT scan at one week showed collapse of the diverticulum and improvement in inflammatory changes (image 5, 6). The patient was discharged with oral antibiotics. At 3month follow-up she was totally asymptomatic with normal liver enzymes. She was counseled regarding potential recurrence and possibility of small intestinal bacterial overgrowth.
Discussion: Small bowel diverticula are of two types, congenital or acquired. They are often found in the second portion of the duodenum adjacent to the ampulla of Vater and are usually asymptomatic but can predispose to choledocholithiasis due to associated biliary dysmotility and papillary dysfunction. Occasionally, an impacted diverticulum can be infected causing diverticulitis such as the case presented and at times even perforation. This case highlights the success of conservative management with antibiotics and endoscopic lavage upon prompt recognition and treatment avoiding invasive measures.

Figure: Image 1: Prominent duodenal diverticulum in the second portion of the duodenum, measuring 3.8 x 2.3 x 2.5 cm.
Image 2: Redemonstration of a relatively large duodenal diverticulum emanating from the second portion of the duodenum with generalized body wall edema.
Image 3: Diverticulum impacted with solid food debris and frank pus emerging
from the diverticulum.
Image 4: A non-bleeding diverticulum, significant improvement in prior inflammation and purulent drainage from last exam.
Image 5, 6: Thickening of the wall of the diverticulum with mucosal enhancement and mild adjacent inflammatory changes.
Image 2: Redemonstration of a relatively large duodenal diverticulum emanating from the second portion of the duodenum with generalized body wall edema.
Image 3: Diverticulum impacted with solid food debris and frank pus emerging
from the diverticulum.
Image 4: A non-bleeding diverticulum, significant improvement in prior inflammation and purulent drainage from last exam.
Image 5, 6: Thickening of the wall of the diverticulum with mucosal enhancement and mild adjacent inflammatory changes.
Disclosures:
Ayesha Khan indicated no relevant financial relationships.
Kian Abdul-Baki indicated no relevant financial relationships.
Keegan Colletier indicated no relevant financial relationships.
Douglas Tyler indicated no relevant financial relationships.
Alexander Perez indicated no relevant financial relationships.
Maryamnaz Falamaki indicated no relevant financial relationships.
Sreeram Parupudi indicated no relevant financial relationships.
Ayesha Khan, DO1, Kian Abdul-Baki, DO1, Keegan Colletier, MD2, Douglas Tyler, MD1, Alexander Perez, MD3, Maryamnaz Falamaki, MD4, Sreeram Parupudi, MD1. P2661 - Periampullary Duodenal Diverticulitis - Another Cause for Acute Pancreatitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
