Monday Poster Session
Category: Small Intestine
P2669 - Not Your Typical Case of Terminal Ileitis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- JS
Jonathan Selzman, DO
University of Texas Health Science Center at San Antonio
San Antonio, TX
Presenting Author(s)
Award: Presidential Poster Award
Jonathan Selzman, DO1, Mahesh Gajendran, MD, MPH1, Benjamin Heriford, DO1, Hamza Khan, MD2, Priyadarshini Loganathan, MD3, Elizabeth Coss, MD1
1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2UT Health San Antonio, San Antonio, TX; 3University of Texas Health Science Center, San Antonio, TX
Introduction: IgA vasculitis is an immune-mediated vasculitis due to IgA deposition. Commonly, this presents with skin and articular symptoms but rarely manifests with significant gastrointestinal (GI) symptoms. We present a rare case of abdominal pain and hematochezia due to IgA Ileitis.
Case Description/Methods: A 58-year-old male with a history of IgA Multiple Myeloma (MM) in remission previously treated with chemotherapy and autologous stem cell transplant presented with days of abdominal pain with nausea. He had one episode of hematochezia days prior to the presentation. He reported finishing a steroid taper one month before the presentation for leukocytoclastic vasculitis (LV). Computed tomography (CT) of the abdomen showed wall thickening of the distal ileum with adjacent fat stranding compatible with distal ileitis. He underwent a colonoscopy which showed congested, erythematous, edematous, granular mucosa in the distal ileum, but these findings were not highly suggestive of Crohn’s disease. The biopsy of the distal ileum revealed acute inflammation in the lamina propria with extravasated red blood cells (RBC) and platelet clumping in/around the capillary vasculature, suggestive of capillaritis. There was no evidence of fibrin thrombi, fibrinoid necrosis of the vessel wall, or leukocytoclasis. The stains for CMV, HSV, AFB, and GMS were negative. Additional immunohistochemical stains showed a positive IgA staining pattern. Altogether, these findings were suggestive of IgA vasculitis. The patient was treated with steroids and had a resolution in the GI symptoms. The bone marrow biopsy showed a relapse of multiple myeloma, and he was started on chemotherapy. Future CT abdomen obtained showed complete resolution of the ileitis with the treatment of MM.
Discussion: While IgA vasculitis is common to manifest with purpuric rash and oligoarticular arthralgias, GI manifestations may present, including abdominal pain and GI bleeding. It is hypothesized that the deposition of IgA complexes leads to submucosal hemorrhage and edema within the GI tract. The presentation may mimic inflammatory bowel disease or infectious gastroenteritis, so endoscopic evaluation and biopsy are important for differentiation. LV commonly affects the small capillaries within the lamina propria. Additionally, the biopsy can reveal lamina propria hemorrhage with RBC sludging and nuclear debris. IgA ileitis should be included in the differential diagnosis in a patient presenting with hematochezia with a known history of Multiple Myeloma.

Disclosures:
Jonathan Selzman, DO1, Mahesh Gajendran, MD, MPH1, Benjamin Heriford, DO1, Hamza Khan, MD2, Priyadarshini Loganathan, MD3, Elizabeth Coss, MD1. P2669 - Not Your Typical Case of Terminal Ileitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Jonathan Selzman, DO1, Mahesh Gajendran, MD, MPH1, Benjamin Heriford, DO1, Hamza Khan, MD2, Priyadarshini Loganathan, MD3, Elizabeth Coss, MD1
1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2UT Health San Antonio, San Antonio, TX; 3University of Texas Health Science Center, San Antonio, TX
Introduction: IgA vasculitis is an immune-mediated vasculitis due to IgA deposition. Commonly, this presents with skin and articular symptoms but rarely manifests with significant gastrointestinal (GI) symptoms. We present a rare case of abdominal pain and hematochezia due to IgA Ileitis.
Case Description/Methods: A 58-year-old male with a history of IgA Multiple Myeloma (MM) in remission previously treated with chemotherapy and autologous stem cell transplant presented with days of abdominal pain with nausea. He had one episode of hematochezia days prior to the presentation. He reported finishing a steroid taper one month before the presentation for leukocytoclastic vasculitis (LV). Computed tomography (CT) of the abdomen showed wall thickening of the distal ileum with adjacent fat stranding compatible with distal ileitis. He underwent a colonoscopy which showed congested, erythematous, edematous, granular mucosa in the distal ileum, but these findings were not highly suggestive of Crohn’s disease. The biopsy of the distal ileum revealed acute inflammation in the lamina propria with extravasated red blood cells (RBC) and platelet clumping in/around the capillary vasculature, suggestive of capillaritis. There was no evidence of fibrin thrombi, fibrinoid necrosis of the vessel wall, or leukocytoclasis. The stains for CMV, HSV, AFB, and GMS were negative. Additional immunohistochemical stains showed a positive IgA staining pattern. Altogether, these findings were suggestive of IgA vasculitis. The patient was treated with steroids and had a resolution in the GI symptoms. The bone marrow biopsy showed a relapse of multiple myeloma, and he was started on chemotherapy. Future CT abdomen obtained showed complete resolution of the ileitis with the treatment of MM.
Discussion: While IgA vasculitis is common to manifest with purpuric rash and oligoarticular arthralgias, GI manifestations may present, including abdominal pain and GI bleeding. It is hypothesized that the deposition of IgA complexes leads to submucosal hemorrhage and edema within the GI tract. The presentation may mimic inflammatory bowel disease or infectious gastroenteritis, so endoscopic evaluation and biopsy are important for differentiation. LV commonly affects the small capillaries within the lamina propria. Additionally, the biopsy can reveal lamina propria hemorrhage with RBC sludging and nuclear debris. IgA ileitis should be included in the differential diagnosis in a patient presenting with hematochezia with a known history of Multiple Myeloma.

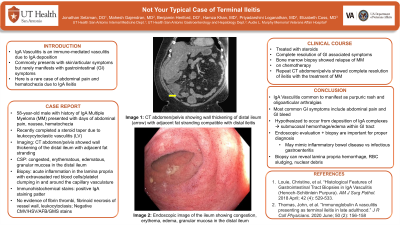
Figure: Figure 1: The computed tomography of the abdomen showing wall thickening of the distal ileum (arrow) with adjacent fat stranding compatible with distal ileitis.
Figure 2: The endoscopic image of the ileum during colonoscopy showing congestion, erythema, edema, and granular mucosa in the distal ileum.
Figure 2: The endoscopic image of the ileum during colonoscopy showing congestion, erythema, edema, and granular mucosa in the distal ileum.
Disclosures:
Jonathan Selzman indicated no relevant financial relationships.
Mahesh Gajendran indicated no relevant financial relationships.
Benjamin Heriford indicated no relevant financial relationships.
Hamza Khan indicated no relevant financial relationships.
Priyadarshini Loganathan indicated no relevant financial relationships.
Elizabeth Coss indicated no relevant financial relationships.
Jonathan Selzman, DO1, Mahesh Gajendran, MD, MPH1, Benjamin Heriford, DO1, Hamza Khan, MD2, Priyadarshini Loganathan, MD3, Elizabeth Coss, MD1. P2669 - Not Your Typical Case of Terminal Ileitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

