Monday Poster Session
Category: Small Intestine
P2673 - Malignant Dysphagia Due to Paraesophageal Metastasis From Ampullary Adenocarcinoma: A Rare Presentation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Alexandra E. Thomson, MD, MPH
HCA Memorial Health University Medical Center
Savannah, GA
Presenting Author(s)
Alexandra E. Thomson, MD, MPH1, Kathleen Humkey, MD1, William Jones, MD1, Daniel Mullady, MD, FACG2
1HCA Memorial Health University Medical Center, Savannah, GA; 2Center for Digestive and Liver Health, Savannah, GA
Introduction: Ampullary adenocarcinomas (AAC) account for approximately 0.2% of gastrointestinal cancers. Typical treatment for early stage disease is pancreatoduodenectomy (PD) and adjuvant chemoradiation (ACR). Metastasis in early stage AAC treated with PD and ACR is rare. Recurrent AAC most commonly occurs in locoregional lymph nodes or metastasis to liver, peritoneum, and bone. We present an unusual case of malignant dysphagia due to mediastinal metastasis from AAC.
Case Description/Methods: A 67-year-old male presented with progressive dysphagia 18 months after PD and ACR for pT2N0M0, G1 AAC. Esophagogastroduodenoscopy (EGD) demonstrated a stricture in the cervical esophagus 20 cm from the incisors. The lumen was severely narrowed to approximately 3 mm with normal mucosa suggesting extrinsic compression or an infiltrative intramural process. Mucosal biopsies were negative for malignancy. PET/CT scan identified focal hypermetabolic activity within an enlarged left paraesophageal lymph node as well as uptake in the surgical bed. Carcinoembrionic antigen-19 (CA19-9) was 714. This was concerning for local recurrence as well as mediastinal metastasis. An endoscopic ultrasound (EUS) was performed for further evaluation and histologic diagnosis confirming the clinical impression of late metastasis from ACC. At the site of the stricture, with wall thickening of 9 mm, predominantly involving submucosa and muscularis propria along with a paraesophageal nodule measuring 15 mm, suspected to be a lymph node. Fine-needle biopsy of the paraesophageal nodule revealed irregular glands with hyperchromatic nuclei on a desmoplastic background consistent pancreatobiliary primary and similar in histologic appearance to the primary ampullary adenocarcinoma. Patient underwent palliative chemoradiation and palliative esophageal stent placement. He passed away from disease progression 1 year after AAC recurrence.
Discussion: This case illustrates late metastasis of early stage ampullary adenocarcinoma after surgical resection and adjuvant chemoradiation to a paraesophageal lymph node resulting in a severe esophageal stricture. Most metastatic disease involves the liver or remote intraperitoneal structures. Distant recurrence of AAC has been reported to the lungs, not within the mediastinum. This pattern of metastasis and resultant malignant dysphagia has not been described in the current literature. Additionally, this case highlights the utility of EUS-directed biopsies of extrinsic strictures of the gastrointestinal tract.

Disclosures:
Alexandra E. Thomson, MD, MPH1, Kathleen Humkey, MD1, William Jones, MD1, Daniel Mullady, MD, FACG2. P2673 - Malignant Dysphagia Due to Paraesophageal Metastasis From Ampullary Adenocarcinoma: A Rare Presentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1HCA Memorial Health University Medical Center, Savannah, GA; 2Center for Digestive and Liver Health, Savannah, GA
Introduction: Ampullary adenocarcinomas (AAC) account for approximately 0.2% of gastrointestinal cancers. Typical treatment for early stage disease is pancreatoduodenectomy (PD) and adjuvant chemoradiation (ACR). Metastasis in early stage AAC treated with PD and ACR is rare. Recurrent AAC most commonly occurs in locoregional lymph nodes or metastasis to liver, peritoneum, and bone. We present an unusual case of malignant dysphagia due to mediastinal metastasis from AAC.
Case Description/Methods: A 67-year-old male presented with progressive dysphagia 18 months after PD and ACR for pT2N0M0, G1 AAC. Esophagogastroduodenoscopy (EGD) demonstrated a stricture in the cervical esophagus 20 cm from the incisors. The lumen was severely narrowed to approximately 3 mm with normal mucosa suggesting extrinsic compression or an infiltrative intramural process. Mucosal biopsies were negative for malignancy. PET/CT scan identified focal hypermetabolic activity within an enlarged left paraesophageal lymph node as well as uptake in the surgical bed. Carcinoembrionic antigen-19 (CA19-9) was 714. This was concerning for local recurrence as well as mediastinal metastasis. An endoscopic ultrasound (EUS) was performed for further evaluation and histologic diagnosis confirming the clinical impression of late metastasis from ACC. At the site of the stricture, with wall thickening of 9 mm, predominantly involving submucosa and muscularis propria along with a paraesophageal nodule measuring 15 mm, suspected to be a lymph node. Fine-needle biopsy of the paraesophageal nodule revealed irregular glands with hyperchromatic nuclei on a desmoplastic background consistent pancreatobiliary primary and similar in histologic appearance to the primary ampullary adenocarcinoma. Patient underwent palliative chemoradiation and palliative esophageal stent placement. He passed away from disease progression 1 year after AAC recurrence.
Discussion: This case illustrates late metastasis of early stage ampullary adenocarcinoma after surgical resection and adjuvant chemoradiation to a paraesophageal lymph node resulting in a severe esophageal stricture. Most metastatic disease involves the liver or remote intraperitoneal structures. Distant recurrence of AAC has been reported to the lungs, not within the mediastinum. This pattern of metastasis and resultant malignant dysphagia has not been described in the current literature. Additionally, this case highlights the utility of EUS-directed biopsies of extrinsic strictures of the gastrointestinal tract.

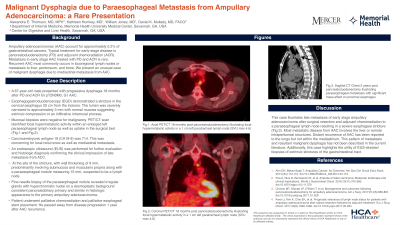
Figure: Figure 1. PET/CT 18 months post pancreatoduodenectomy illustrating focal hypermetabolic activity in a 1 cm left paratracheal lymph node (SVU max 4.6) axial (A) and coronal (B) images. CT Chest 2 years post pancreatoduodenectomy illustrating paraesophageal metastasis with significant mass effect on proximal esophagus (arrow) sagittal image (C).
Disclosures:
Alexandra Thomson indicated no relevant financial relationships.
Kathleen Humkey indicated no relevant financial relationships.
William Jones indicated no relevant financial relationships.
Daniel Mullady indicated no relevant financial relationships.
Alexandra E. Thomson, MD, MPH1, Kathleen Humkey, MD1, William Jones, MD1, Daniel Mullady, MD, FACG2. P2673 - Malignant Dysphagia Due to Paraesophageal Metastasis From Ampullary Adenocarcinoma: A Rare Presentation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

