Monday Poster Session
Category: Small Intestine
P2674 - A Unique Case of Goblet Cell Adenocarcinoma Mimicking Crohn's Disease
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Talha M. Qureshi, MD
Rockford Gastroenterology Associates
Rockford, IL
Presenting Author(s)
Talha M. Qureshi, MD, Ilche Nonevski, MD
Rockford Gastroenterology Associates, Rockford, IL
Introduction: Appendiceal goblet cell adenocarcinoma (GCA) is among the rarest tumors with an incidence reported at 0.05 cases per 100,000. There have only been 369 cases reported over a 30 year span from the 1970s. Even though these tumors stain positive for neuroendocrine markers, they behave more aggressively like conventional adenocarcinomas. GCA most commonly presents as appendicitis and is discovered incidentally after appendectomy. This case reports a unique presentation of GCA behaving like Crohns disease and an interesting management outcome.
Case Description/Methods: A 60-year-old male presented with two months of intermittent RLQ pain and weight loss. He denied any diarrhea or blood in the stools. Vital signs were within normal limits. On exam, he was noted to have abdominal distention and RLQ tenderness. Labs were significant for hematocrit of 37.8% and CRP of 0.13 mg/dl. CT scan showed irregular thickening at the ileoceal valve and cecum with proximal dilation of the small bowel consistent with small bowel obstruction (SBO). Initial management involved IVF, NPO, and NG tube decompression without success. Empiric treatment of suspected Crohns was initiated with methylprednisone. Steroids were successful and patient was able to prep for a colonoscopy. On colonoscopy, he was found to have an ulcerated, polypoid-appearing lesion at the appendiceal orifice. There was stenosis at ileocecal junction not allowing for ileal intubation. Pathology of the appendiceal orifice confirmed the diagnosis of GCA. There was no evidence of distant metastases and he underwent a right hemicolectomy two weeks later with 9/13 lymph nodes positive for adenocarcinoma.
Discussion: This case presents a unique clinical dilemma of GCA presenting with an SBO in the setting of imaging concerning for a Crohns stricture. Most cases of appendiceal GCA in the literature involve initial, limited surgical resection, often requiring additional surgery after confirming the diagnosis on pathology. The use of empiric steroids in this case allowed for clinical resolution of symptoms and rare colonoscopic diagnosis of GCA. It is reported that 20-40% of adenocarcinomas in the colon may have an inflammatory component suggesting the prompt resolution after steroids. This management outcome allowed for appropriate staging and surgical management of GCA which behaves similarly to colon adenocarcinomas. This case raises awareness of a rare appendiceal tumor mimicking a Crohns stricture and how empiric steroid use resulted in improved morbidity.

Disclosures:
Talha M. Qureshi, MD, Ilche Nonevski, MD. P2674 - A Unique Case of Goblet Cell Adenocarcinoma Mimicking Crohn's Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Rockford Gastroenterology Associates, Rockford, IL
Introduction: Appendiceal goblet cell adenocarcinoma (GCA) is among the rarest tumors with an incidence reported at 0.05 cases per 100,000. There have only been 369 cases reported over a 30 year span from the 1970s. Even though these tumors stain positive for neuroendocrine markers, they behave more aggressively like conventional adenocarcinomas. GCA most commonly presents as appendicitis and is discovered incidentally after appendectomy. This case reports a unique presentation of GCA behaving like Crohns disease and an interesting management outcome.
Case Description/Methods: A 60-year-old male presented with two months of intermittent RLQ pain and weight loss. He denied any diarrhea or blood in the stools. Vital signs were within normal limits. On exam, he was noted to have abdominal distention and RLQ tenderness. Labs were significant for hematocrit of 37.8% and CRP of 0.13 mg/dl. CT scan showed irregular thickening at the ileoceal valve and cecum with proximal dilation of the small bowel consistent with small bowel obstruction (SBO). Initial management involved IVF, NPO, and NG tube decompression without success. Empiric treatment of suspected Crohns was initiated with methylprednisone. Steroids were successful and patient was able to prep for a colonoscopy. On colonoscopy, he was found to have an ulcerated, polypoid-appearing lesion at the appendiceal orifice. There was stenosis at ileocecal junction not allowing for ileal intubation. Pathology of the appendiceal orifice confirmed the diagnosis of GCA. There was no evidence of distant metastases and he underwent a right hemicolectomy two weeks later with 9/13 lymph nodes positive for adenocarcinoma.
Discussion: This case presents a unique clinical dilemma of GCA presenting with an SBO in the setting of imaging concerning for a Crohns stricture. Most cases of appendiceal GCA in the literature involve initial, limited surgical resection, often requiring additional surgery after confirming the diagnosis on pathology. The use of empiric steroids in this case allowed for clinical resolution of symptoms and rare colonoscopic diagnosis of GCA. It is reported that 20-40% of adenocarcinomas in the colon may have an inflammatory component suggesting the prompt resolution after steroids. This management outcome allowed for appropriate staging and surgical management of GCA which behaves similarly to colon adenocarcinomas. This case raises awareness of a rare appendiceal tumor mimicking a Crohns stricture and how empiric steroid use resulted in improved morbidity.

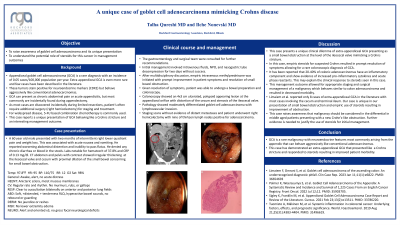
Figure: A. Coronal computed tomography image with contrast showing irregular thickening of the ileocecal valve and cecum. B. Colonoscopy showing polypoid-appearing congested mucosa in the cecum. C. Appendiceal orifice with ulcerated and polypoid-appearing tissue. D. Pathology slide showing amphicrine neoplasm containing goblet-like mucinous cells with endocrine cells and Paneth-like cells arranged in a tubular architecture, resembling intestinal crypts, confirming the diagnosis of goblet cell adenocarcinoma.
Disclosures:
Talha Qureshi indicated no relevant financial relationships.
Ilche Nonevski indicated no relevant financial relationships.
Talha M. Qureshi, MD, Ilche Nonevski, MD. P2674 - A Unique Case of Goblet Cell Adenocarcinoma Mimicking Crohn's Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

