Monday Poster Session
Category: Small Intestine
P2676 - Diffuse Intestinal Edema and Possible Intestinal Vasculitis as Manifestations of Sjogren’s Syndrome
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Fangfang Wang, MD
Mayo Clinic Arizona
Phoenix, AZ
Presenting Author(s)
Fangfang Wang, MD1, Michael Pham, MD2, Nelly Tan, 2, Gassan Kassim, MD2, Jennifer L. Horsley-Silva, MD1
1Mayo Clinic Arizona, Phoenix, AZ; 2Mayo Clinic Arizona, Scottsdale, AZ
Introduction: Sjogren’s syndrome (SS) is an infiltrative autoimmune disorder that primarily affects exocrine glands. Gastrointestinal (GI) manifestations associated with SS have been documented, including gastritis, duodenal ulcers, GI dysmotility, primary biliary cholangitis, autoimmune hepatitis, pancreatitis, celiac disease, and mesenteric panniculitis. This case report presents a unique instance of diffuse bowel edema in a patient diagnosed with possible intestinal vasculitis associated with SS.
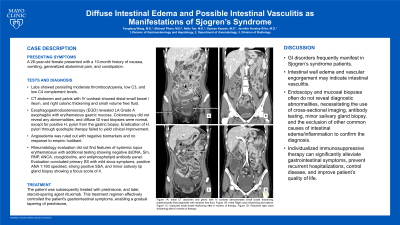
Case Description/Methods: A 26-year-old female presented with a 10-month history of nausea, vomiting, generalized abdominal pain, and constipation. Labs showed persisting moderate thrombocytopenia, low C3, and low C4 complement levels. CT abdomen and pelvis with IV contrast showed distal small bowel / ileum, and right colonic thickening and small volume free fluid. Esophagogastroduodenoscopy (EGD) revealed LA Grade A esophagitis with erythematous gastric mucosa. Colonoscopy did not reveal any abnormalities, and diffuse GI tract biopsies were normal, except for positive H. pylori from the gastric biopsy. Eradication of H. pylori through quadruple therapy failed to yield clinical improvement. Angioedema was ruled out with negative biomarkers and no response to empiric Icatibant. Rheumatology evaluation did not find features of systemic lupus erythematosus with additional testing showing negative dsDNA, Sm, RNP, ANCA, cryoglobulins, and antiphospholipid antibody panel. Evaluation concluded primary SS with mild sicca symptoms, positive ANA 1:160 speckled, strong positive SSA, and minor salivary lip gland biopsy showing a focus score of 4. The patient was subsequently treated with prednisone, and later, steroid-sparing agent rituximab. This treatment regimen effectively controlled the patient's gastrointestinal symptoms, enabling a gradual tapering of prednisone, and normalization complements and thrombocytopenia.
Discussion: GI disorders frequently manifest in SS patients. Intestinal wall edema and vascular engorgement may indicate intestinal vasculitis. Endoscopy and mucosal biopsies often do not reveal diagnostic abnormalities, necessitating the use of cross-sectional imaging, antibody testing, minor salivary gland biopsy, and the exclusion of other common causes of intestinal edema/inflammation to confirm the diagnosis. Individualized immunosuppressive therapy can significantly alleviate gastrointestinal symptoms, prevent recurrent hospitalizations, control disease, and improve patient’s quality of life.

Disclosures:
Fangfang Wang, MD1, Michael Pham, MD2, Nelly Tan, 2, Gassan Kassim, MD2, Jennifer L. Horsley-Silva, MD1. P2676 - Diffuse Intestinal Edema and Possible Intestinal Vasculitis as Manifestations of Sjogren’s Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mayo Clinic Arizona, Phoenix, AZ; 2Mayo Clinic Arizona, Scottsdale, AZ
Introduction: Sjogren’s syndrome (SS) is an infiltrative autoimmune disorder that primarily affects exocrine glands. Gastrointestinal (GI) manifestations associated with SS have been documented, including gastritis, duodenal ulcers, GI dysmotility, primary biliary cholangitis, autoimmune hepatitis, pancreatitis, celiac disease, and mesenteric panniculitis. This case report presents a unique instance of diffuse bowel edema in a patient diagnosed with possible intestinal vasculitis associated with SS.
Case Description/Methods: A 26-year-old female presented with a 10-month history of nausea, vomiting, generalized abdominal pain, and constipation. Labs showed persisting moderate thrombocytopenia, low C3, and low C4 complement levels. CT abdomen and pelvis with IV contrast showed distal small bowel / ileum, and right colonic thickening and small volume free fluid. Esophagogastroduodenoscopy (EGD) revealed LA Grade A esophagitis with erythematous gastric mucosa. Colonoscopy did not reveal any abnormalities, and diffuse GI tract biopsies were normal, except for positive H. pylori from the gastric biopsy. Eradication of H. pylori through quadruple therapy failed to yield clinical improvement. Angioedema was ruled out with negative biomarkers and no response to empiric Icatibant. Rheumatology evaluation did not find features of systemic lupus erythematosus with additional testing showing negative dsDNA, Sm, RNP, ANCA, cryoglobulins, and antiphospholipid antibody panel. Evaluation concluded primary SS with mild sicca symptoms, positive ANA 1:160 speckled, strong positive SSA, and minor salivary lip gland biopsy showing a focus score of 4. The patient was subsequently treated with prednisone, and later, steroid-sparing agent rituximab. This treatment regimen effectively controlled the patient's gastrointestinal symptoms, enabling a gradual tapering of prednisone, and normalization complements and thrombocytopenia.
Discussion: GI disorders frequently manifest in SS patients. Intestinal wall edema and vascular engorgement may indicate intestinal vasculitis. Endoscopy and mucosal biopsies often do not reveal diagnostic abnormalities, necessitating the use of cross-sectional imaging, antibody testing, minor salivary gland biopsy, and the exclusion of other common causes of intestinal edema/inflammation to confirm the diagnosis. Individualized immunosuppressive therapy can significantly alleviate gastrointestinal symptoms, prevent recurrent hospitalizations, control disease, and improve patient’s quality of life.

Figure: Figure 1A: Initial CT abdomen and pelvis with IV contrast demonstrates small bowel thickening, predominantly ileal segments with reactive free fluid.
Figure 1B: Initial Right colon thickening and edema.
Figure 1C: Improved small bowel thickening after 6 months of therapy.
Figure 1D: Resolved right colon thickening after 6 months of therapy
Figure 1B: Initial Right colon thickening and edema.
Figure 1C: Improved small bowel thickening after 6 months of therapy.
Figure 1D: Resolved right colon thickening after 6 months of therapy
Disclosures:
Fangfang Wang indicated no relevant financial relationships.
Michael Pham indicated no relevant financial relationships.
Nelly Tan indicated no relevant financial relationships.
Gassan Kassim indicated no relevant financial relationships.
Jennifer Horsley-Silva: Regeneron – Advisory Committee/Board Member, Independent Contractor. Sanofi – Advisory Committee/Board Member.
Fangfang Wang, MD1, Michael Pham, MD2, Nelly Tan, 2, Gassan Kassim, MD2, Jennifer L. Horsley-Silva, MD1. P2676 - Diffuse Intestinal Edema and Possible Intestinal Vasculitis as Manifestations of Sjogren’s Syndrome, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
