Monday Poster Session
Category: Small Intestine
P2684 - Presence of Portomesenteric Venous Gas and Pneumatosis Intestinalis in Nonocclusive Mesenteric Ischemia as a Complication of Transrectal Ultrasound-Guided Prostate Biopsy
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Nazli Begum Ozturk, MD
Beaumont Hospital
Royal Oak, MI
Presenting Author(s)
Nazli Begum Ozturk, MD1, Ayca Zeynep Kutlu, MD2, Raim Iliaz, MD3
1Beaumont Hospital, Royal Oak, MI; 2University of Wisconsin-Madison, Madison, WI; 3Atlas University, Istanbul, Istanbul, Turkey
Introduction: Transrectal ultrasound (TRUS)-guided prostate biopsy is a common and safe procedure with mild and self-limiting post-biopsy complications. Nonocclusive mesenteric ischemia (NOMI), or ischemic colitis if only colon is involved, is seen due to intestinal hypoperfusion. In this case, we report a patient with hemorrhagic shock and NOMI with computed tomography (CT) imaging findings of pneumatosis intestinalis (PI) and portomesenteric venous gas (PMVG) post-TRUS-guided prostate biopsy.
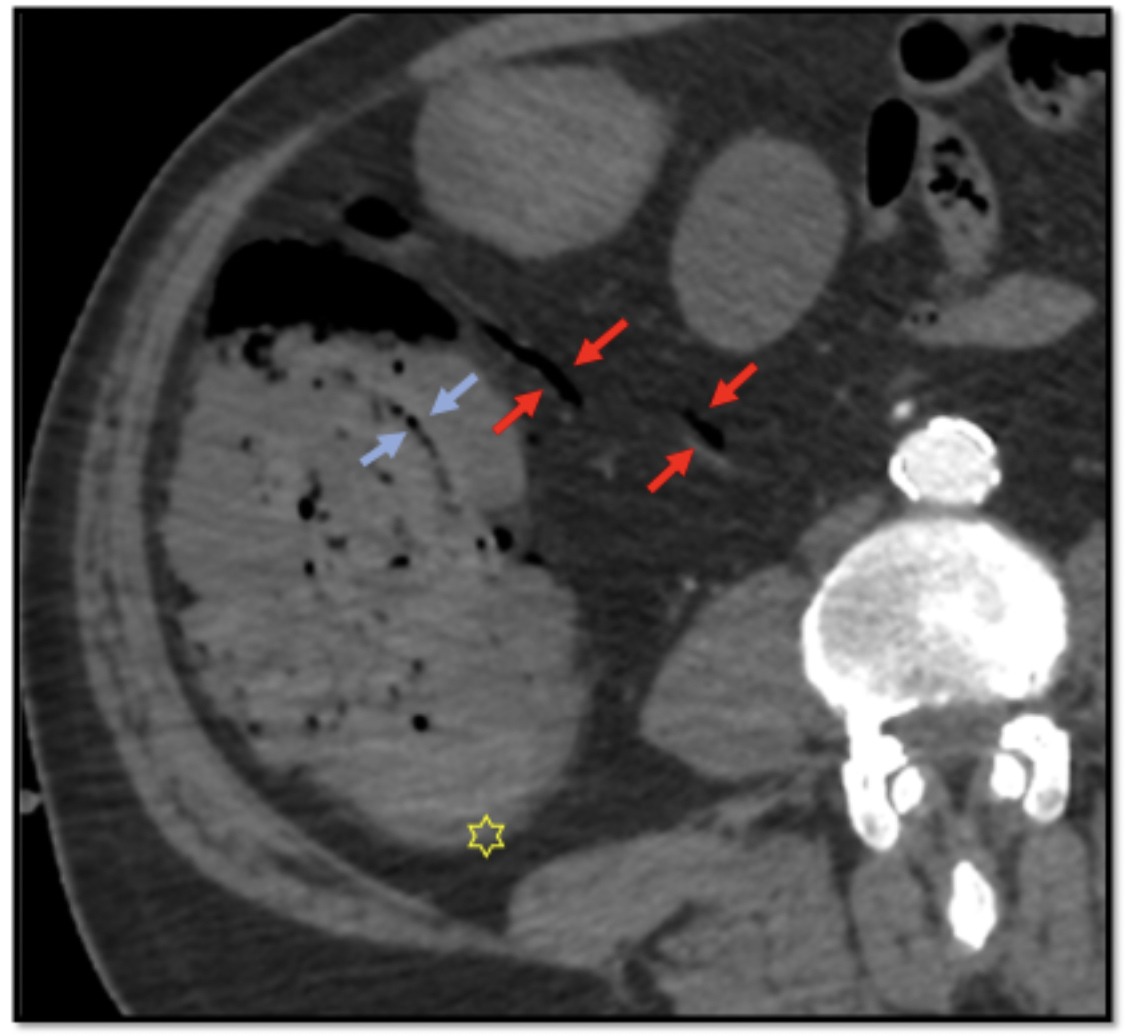
Case Description/Methods: A 58-year-old man presented to the emergency department with bright red blood per rectum, fatigue, and lightheadedness. He had a medical history significant for mechanical aortic valve replacement and was on warfarin. He underwent TRUS-guided prostate biopsy for concerns of prostate cancer five days prior to his presentation. Patient was hypotensive at 95/55 mmHg and tachycardic at 116 bpm on presentation. Laboratory work-up was remarkable for WBC:11.2, Hgb: 6.6, Plt: 247, INR: 1.07. Large-volume fluid resuscitation, packed red blood cell transfusion, and empiric broad-spectrum intravenous (IV) antibiotic therapy were initiated and the patient was admitted to the intensive care unit for management of hemorrhagic shock. IV contrast-enhanced abdominopelvic CT demonstrated ascending colon wall thickening, PMVG, and PI. A colonoscopy was performed and circular ischemic ulcers at the ascending colon were found. Furthermore, stigmata of recent bleeding was found in the rectum at the former biopsy site and was treated endoscopically. Patient was discharged home following continued improvement during hospitalization. A repeat colonoscopy at week 8 showed the presence of one 8-9 mm clean-based ulcer and one ulcer at healing process at the ascending colon. Patient continued to be symptom free and did not experience recurrent bleeding.
Discussion: PI and PVMG are radiologic signs that are nonspecific and can be seen in both benign and life-threatening conditions. CT findings of concomitant PI and PMVG is usually seen in the setting of mesenteric infarction, however both PI and PMVG may or may not be present in NOMI. As these signs can be seen in benign conditions, they should not be always interpreted as ominous signs, but rather should be interpreted within appropriate clinical context.
Disclosures:
Nazli Begum Ozturk, MD1, Ayca Zeynep Kutlu, MD2, Raim Iliaz, MD3. P2684 - Presence of Portomesenteric Venous Gas and Pneumatosis Intestinalis in Nonocclusive Mesenteric Ischemia as a Complication of Transrectal Ultrasound-Guided Prostate Biopsy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Beaumont Hospital, Royal Oak, MI; 2University of Wisconsin-Madison, Madison, WI; 3Atlas University, Istanbul, Istanbul, Turkey
Introduction: Transrectal ultrasound (TRUS)-guided prostate biopsy is a common and safe procedure with mild and self-limiting post-biopsy complications. Nonocclusive mesenteric ischemia (NOMI), or ischemic colitis if only colon is involved, is seen due to intestinal hypoperfusion. In this case, we report a patient with hemorrhagic shock and NOMI with computed tomography (CT) imaging findings of pneumatosis intestinalis (PI) and portomesenteric venous gas (PMVG) post-TRUS-guided prostate biopsy.
Case Description/Methods: A 58-year-old man presented to the emergency department with bright red blood per rectum, fatigue, and lightheadedness. He had a medical history significant for mechanical aortic valve replacement and was on warfarin. He underwent TRUS-guided prostate biopsy for concerns of prostate cancer five days prior to his presentation. Patient was hypotensive at 95/55 mmHg and tachycardic at 116 bpm on presentation. Laboratory work-up was remarkable for WBC:11.2, Hgb: 6.6, Plt: 247, INR: 1.07. Large-volume fluid resuscitation, packed red blood cell transfusion, and empiric broad-spectrum intravenous (IV) antibiotic therapy were initiated and the patient was admitted to the intensive care unit for management of hemorrhagic shock. IV contrast-enhanced abdominopelvic CT demonstrated ascending colon wall thickening, PMVG, and PI. A colonoscopy was performed and circular ischemic ulcers at the ascending colon were found. Furthermore, stigmata of recent bleeding was found in the rectum at the former biopsy site and was treated endoscopically. Patient was discharged home following continued improvement during hospitalization. A repeat colonoscopy at week 8 showed the presence of one 8-9 mm clean-based ulcer and one ulcer at healing process at the ascending colon. Patient continued to be symptom free and did not experience recurrent bleeding.
Discussion: PI and PVMG are radiologic signs that are nonspecific and can be seen in both benign and life-threatening conditions. CT findings of concomitant PI and PMVG is usually seen in the setting of mesenteric infarction, however both PI and PMVG may or may not be present in NOMI. As these signs can be seen in benign conditions, they should not be always interpreted as ominous signs, but rather should be interpreted within appropriate clinical context.
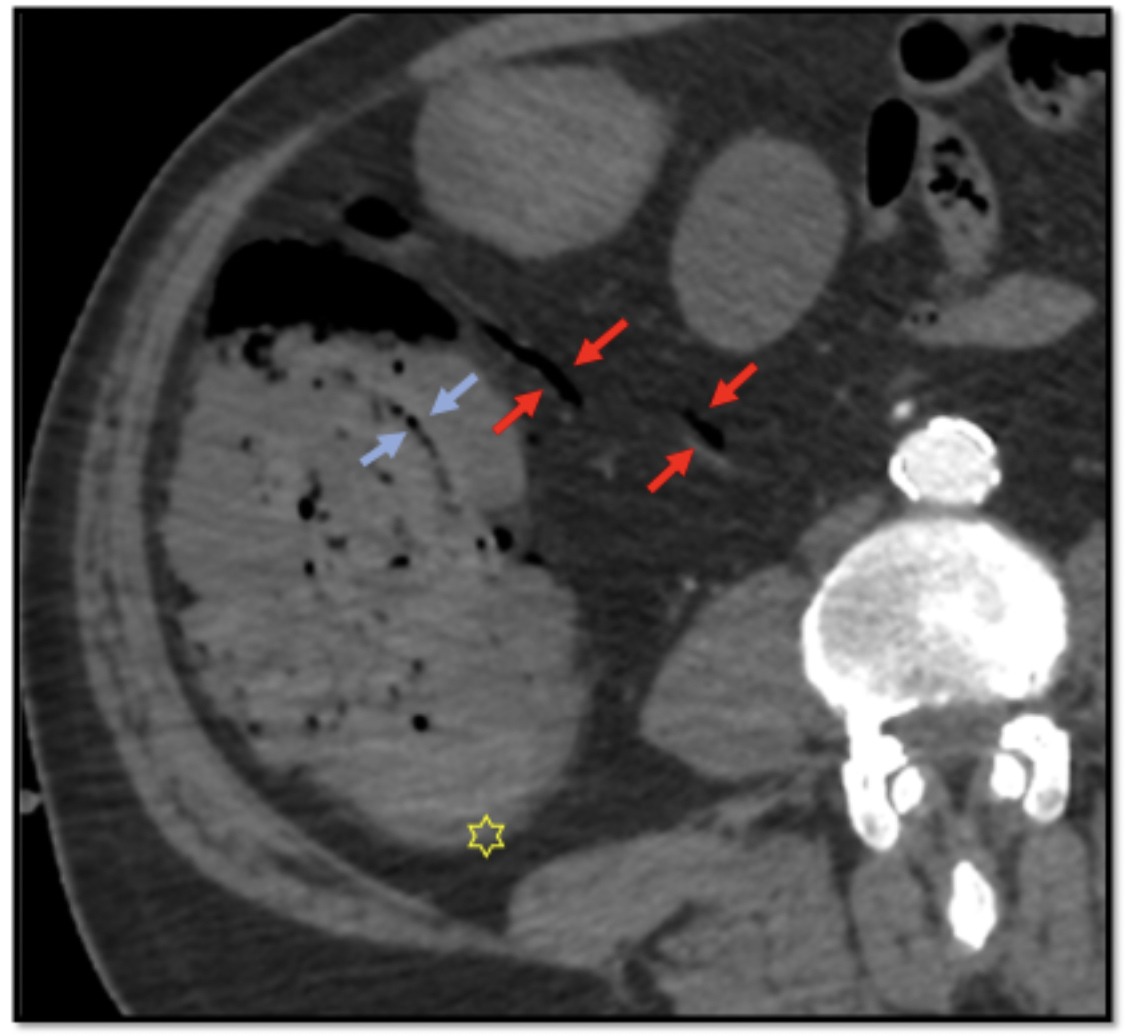
Figure: Axial slice of contrast-enhanced abdominopelvic CT demonstrates ascending colon wall thickening (yellow star), portomesenteric venous gas (red arrows), and pneumatosis intestinalis (blue arrows).
Disclosures:
Nazli Begum Ozturk indicated no relevant financial relationships.
Ayca Zeynep Kutlu indicated no relevant financial relationships.
Raim Iliaz indicated no relevant financial relationships.
Nazli Begum Ozturk, MD1, Ayca Zeynep Kutlu, MD2, Raim Iliaz, MD3. P2684 - Presence of Portomesenteric Venous Gas and Pneumatosis Intestinalis in Nonocclusive Mesenteric Ischemia as a Complication of Transrectal Ultrasound-Guided Prostate Biopsy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
