Monday Poster Session
Category: Small Intestine
P2685 - Diagnosis of Aortoenteric Fistula: A Case Report
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- KC
Kaitlyn Cronk, MD
University of Mississippi Medical Center
Jackson, Mississippi
Presenting Author(s)
Kaitlyn Cronk, MD, Anna Owings, DO, Shou-Jiang Tang, MD, Himmat Brar, MBBS
University of Mississippi Medical Center, Jackson, MS
Introduction: Aortoenteric fistula (AEF) is a rare cause of gastrointestinal bleeding associated with high mortality. An AEF is defined as an aberrant, direct connection between the aorta and the gastrointestinal (GI) tract. An AEF can be primary or secondary in etiology such as the intrusion of aortic aneurysms with proximal GI anatomy or a post-surgical complication of abdominal aortic aneurysm (AAA) repair, respectively. Here we report a case of an aortoenteric fistula presenting 17 years after AAA repair with an initial symptom of melena.
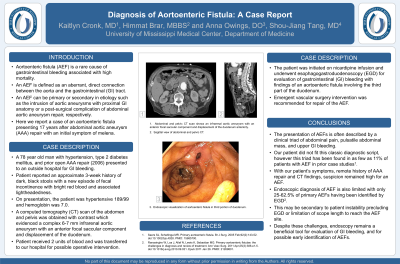
Case Description/Methods: A 78 year old man with hypertension, type 2 diabetes mellitus, and prior open AAA repair (2006) presented to an outside hospital for GI bleeding. Patient reported an approximate 3-week history of dark, black stools with a new episode of fecal incontinence with bright red blood and associated lightheadedness. On presentation, the patient was hypertensive 189/99 and hemoglobin was 7.0. A computed tomography (CT) scan of the abdomen and pelvis was obtained with contrast which evidenced a complex 6-7 mm infrarenal aortic aneurysm with an anterior focal saccular component and displacement of the duodenum. Patient received 2 units of blood and was transferred to our hospital for possible operative intervention. The patient was initiated on nicardipine infusion and underwent esophagogastroduodenoscopy (EGD) for evaluation of GI bleeding with findings of an aortoenteric fistula involving the third part of the duodenum. Emergent vascular surgery intervention was recommended for AEF repair.
Discussion: The presentation of AEFs is often described by a clinical triad of abdominal pain, pulsatile abdominal mass, and upper GI bleeding. Our patient did not fit this classic diagnostic script, however, and this triad has been found in as few as 11% of patients in prior case studies.1 With our patient’s symptoms, remote history of AAA repair and CT findings, suspicion remained high for an AEF. Endoscopic diagnosis of AEF is also limited with only 25-62.5% of primary AEFs having been identified by EGD.2 This may be secondary to patient instability precluding EGD or limitation of scope length to reach the AEF site. Despite these challenges, endoscopy remains a beneficial tool for evaluation of GI bleeding, and for possible early identification of AEFs.
1.Saers SJ, Scheltinga MR. Primary aortoenteric fistula. 2005 Feb. 143-152.
2.Ranasinghe, Weranja et al. Primary aortoenteric fistulae: the challenges in diagnosis and review of treatment. 2011 Apr. 386.e1-5.

Disclosures:
Kaitlyn Cronk, MD, Anna Owings, DO, Shou-Jiang Tang, MD, Himmat Brar, MBBS. P2685 - Diagnosis of Aortoenteric Fistula: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of Mississippi Medical Center, Jackson, MS
Introduction: Aortoenteric fistula (AEF) is a rare cause of gastrointestinal bleeding associated with high mortality. An AEF is defined as an aberrant, direct connection between the aorta and the gastrointestinal (GI) tract. An AEF can be primary or secondary in etiology such as the intrusion of aortic aneurysms with proximal GI anatomy or a post-surgical complication of abdominal aortic aneurysm (AAA) repair, respectively. Here we report a case of an aortoenteric fistula presenting 17 years after AAA repair with an initial symptom of melena.
Case Description/Methods: A 78 year old man with hypertension, type 2 diabetes mellitus, and prior open AAA repair (2006) presented to an outside hospital for GI bleeding. Patient reported an approximate 3-week history of dark, black stools with a new episode of fecal incontinence with bright red blood and associated lightheadedness. On presentation, the patient was hypertensive 189/99 and hemoglobin was 7.0. A computed tomography (CT) scan of the abdomen and pelvis was obtained with contrast which evidenced a complex 6-7 mm infrarenal aortic aneurysm with an anterior focal saccular component and displacement of the duodenum. Patient received 2 units of blood and was transferred to our hospital for possible operative intervention. The patient was initiated on nicardipine infusion and underwent esophagogastroduodenoscopy (EGD) for evaluation of GI bleeding with findings of an aortoenteric fistula involving the third part of the duodenum. Emergent vascular surgery intervention was recommended for AEF repair.
Discussion: The presentation of AEFs is often described by a clinical triad of abdominal pain, pulsatile abdominal mass, and upper GI bleeding. Our patient did not fit this classic diagnostic script, however, and this triad has been found in as few as 11% of patients in prior case studies.1 With our patient’s symptoms, remote history of AAA repair and CT findings, suspicion remained high for an AEF. Endoscopic diagnosis of AEF is also limited with only 25-62.5% of primary AEFs having been identified by EGD.2 This may be secondary to patient instability precluding EGD or limitation of scope length to reach the AEF site. Despite these challenges, endoscopy remains a beneficial tool for evaluation of GI bleeding, and for possible early identification of AEFs.
1.Saers SJ, Scheltinga MR. Primary aortoenteric fistula. 2005 Feb. 143-152.
2.Ranasinghe, Weranja et al. Primary aortoenteric fistulae: the challenges in diagnosis and review of treatment. 2011 Apr. 386.e1-5.

Figure: A. Abdominal and pelvic contrasted computed tomography (CT) scan shows an infrarenal aortic aneurysm with an anterior focal saccular component and displacement of the duodenum anteriorly.
B. Sagittal view of abdominal and pelvic CT.
C. Endoscopic visualization of aortoenteric fistula in third portion of duodenum.
B. Sagittal view of abdominal and pelvic CT.
C. Endoscopic visualization of aortoenteric fistula in third portion of duodenum.
Disclosures:
Kaitlyn Cronk indicated no relevant financial relationships.
Anna Owings indicated no relevant financial relationships.
Shou-Jiang Tang indicated no relevant financial relationships.
Himmat Brar indicated no relevant financial relationships.
Kaitlyn Cronk, MD, Anna Owings, DO, Shou-Jiang Tang, MD, Himmat Brar, MBBS. P2685 - Diagnosis of Aortoenteric Fistula: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
