Monday Poster Session
Category: Small Intestine
P2696 - Pyloric Gland Adenoma Arising Within the Duodenal Bulb
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Luis G. Rendon Rodriguez, MD
Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Luis Rendon Rodriguez, MD1, Bo Hyung Yoon, MD2, Edward Lung, MD, MPH3
1Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction:
Pyloric gland adenomas (PGA) are rare pre-cancerous lesions most often identified in the stomach, but also seen within the esophagus, duodenum, gallbladder, bile ducts, and rectum. Among these, few cases have been identified in the duodenum and even fewer in the duodenal bulb. Additionally, most reported PGAs have been < 25mm. Prompt identification and resection is crucial as the risk of developing into adenocarcinoma increases with size and degree of dysplasia. This is a case report of endoscopic resection using a hot snare of a large duodenal bulb PGA.
Case Description/Methods:
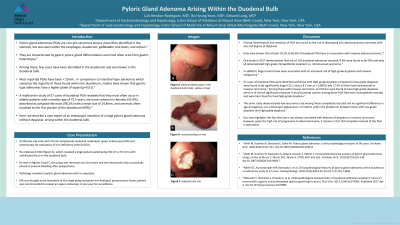
A 80-year-old male with chronic lymphocytic leukemia underwent upper endoscopy (EGD) and colonoscopy for evaluation of iron deficiency anemia (IDA). He underwent EGD which revealed a large pedunculated polyp (50 mm x 65 mm) with umbilicated focus in the duodenal bulb (Figure 1A and 1B). The polyp was completely removed via a hot snare (Figure 1C) and two hemostatic clips successfully placed to prevent bleeding after polypectomy. Pathology revealed a pyloric gland adenoma with no dysplasia. IDA was thought to be secondary to this large polyp and given this finding of precancerous lesion, patient was recommended to repeat an upper endoscopy in one year for surveillance.
Discussion:
Early recognition and swift removal of PGAs are crucial to prevent progression to adenocarcinoma. Larger lesions have been associated with an increased risk of high-grade dysplasia and invasive malignancy. In a study by Miller et al., 57 cases of duodenal PGA were identified and those with high-grade dysplasia compared to low-grade dysplasia were found to be significantly larger (23.1 versus 8.7 mm; p = 0.0001) and 17.9% of them had intramucosal or invasive carcinoma. The same study demonstrated low recurrence rate among those completely resected. Our case highlights the fact that size is not always correlated with features of dysplasia or invasive carcinoma. However, given the high risk of progression to adenocarcinoma, complete removal of the PGA is warranted.

Disclosures:
Luis Rendon Rodriguez, MD1, Bo Hyung Yoon, MD2, Edward Lung, MD, MPH3. P2696 - Pyloric Gland Adenoma Arising Within the Duodenal Bulb, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai, New York, NY; 2Icahn School of Medicine at Mount Sinai, New York, NY; 3Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction:
Pyloric gland adenomas (PGA) are rare pre-cancerous lesions most often identified in the stomach, but also seen within the esophagus, duodenum, gallbladder, bile ducts, and rectum. Among these, few cases have been identified in the duodenum and even fewer in the duodenal bulb. Additionally, most reported PGAs have been < 25mm. Prompt identification and resection is crucial as the risk of developing into adenocarcinoma increases with size and degree of dysplasia. This is a case report of endoscopic resection using a hot snare of a large duodenal bulb PGA.
Case Description/Methods:
A 80-year-old male with chronic lymphocytic leukemia underwent upper endoscopy (EGD) and colonoscopy for evaluation of iron deficiency anemia (IDA). He underwent EGD which revealed a large pedunculated polyp (50 mm x 65 mm) with umbilicated focus in the duodenal bulb (Figure 1A and 1B). The polyp was completely removed via a hot snare (Figure 1C) and two hemostatic clips successfully placed to prevent bleeding after polypectomy. Pathology revealed a pyloric gland adenoma with no dysplasia. IDA was thought to be secondary to this large polyp and given this finding of precancerous lesion, patient was recommended to repeat an upper endoscopy in one year for surveillance.
Discussion:
Early recognition and swift removal of PGAs are crucial to prevent progression to adenocarcinoma. Larger lesions have been associated with an increased risk of high-grade dysplasia and invasive malignancy. In a study by Miller et al., 57 cases of duodenal PGA were identified and those with high-grade dysplasia compared to low-grade dysplasia were found to be significantly larger (23.1 versus 8.7 mm; p = 0.0001) and 17.9% of them had intramucosal or invasive carcinoma. The same study demonstrated low recurrence rate among those completely resected. Our case highlights the fact that size is not always correlated with features of dysplasia or invasive carcinoma. However, given the high risk of progression to adenocarcinoma, complete removal of the PGA is warranted.

Figure: Figure 1A: pedunculated polyp in the duodenal bulb (stalk, yellow arrow), B: resected polyp ex vivo, C: polypectomy site
Disclosures:
Luis Rendon Rodriguez indicated no relevant financial relationships.
Bo Hyung Yoon indicated no relevant financial relationships.
Edward Lung indicated no relevant financial relationships.
Luis Rendon Rodriguez, MD1, Bo Hyung Yoon, MD2, Edward Lung, MD, MPH3. P2696 - Pyloric Gland Adenoma Arising Within the Duodenal Bulb, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
