Monday Poster Session
Category: Small Intestine
P2701 - An Rare Case of Strongyloides Hyperinfection Syndrome as a Manifestation of Immune Reconstituted Inflammatory Syndrome in an HIV-Infected Patient
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- SA
Shuhaib Ali, MD
UT Health San Antonio
San Antonio, TX
Presenting Author(s)
Shuhaib Ali, MD1, Kavea Panneerselvam, MD2, Patrick Snyder, MD2, Juan Echavarria, MD2, Onyinye Okonkwo, MD3
1UT Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center at San Antonio, San Antonio, TX; 3UTHSCSA, San Antonio, TX
Introduction: Strongyloides hyperinfection syndrome (SHS) occurs as a result of accelerated autoinfection in patients who have had a sudden change in their immune status. Here, we present a rare case of SHS as a manifestation of immune reconstitution inflammatory syndrome (IRIS) in a patient with HIV, and unconventional treatment with subcutaneous ivermectin.
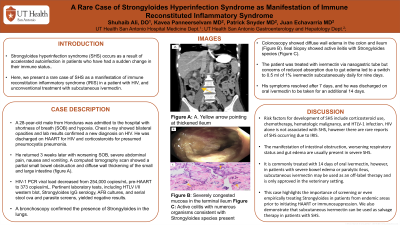
Case Description/Methods: A 28-year-old male from Honduras was admitted to the hospital with shortness of breath (SOB) and hypoxia. Chest x-ray showed bilateral opacities and lab results confirmed a new diagnosis on HIV. He was discharged on HAART for HIV and corticosteroids for presumed pneumocystis pneumonia. He returned 3 weeks later with worsening SOB, severe abdominal pain, nausea and vomiting. A computed tomography scan showed a partial small bowel obstruction and diffuse wall thickening of the small and large intestine (figure A). HIV-1 PCR viral load decreased from 254,000 copies/mL pre-HAART to 373 copies/mL. Pertinent laboratory tests, including HTLV I/II western blot, Strongyloides IgG serology, AFB cultures, and serial stool ova and parasite screens, yielded negative results. A bronchoscopy confirmed the presence of Strongyloides in the lungs. Colonoscopy showed diffuse wall edema in the colon and ileum (Figure B). Ileal biopsy showed active ileitis with Strongyloides species (Figure C). The patient was treated with ivermectin via nasogastric tube, but concerns of reduced absorption due to gut edema led to a switch to 0.5 ml of 1% ivermectin subcutaneously daily for nine days. His symptoms resolved after 7 days and he was discharged on oral ivermectin to be taken for an additional 14 days.
Discussion: Risk factors for development of SHS include corticosteroid use, chemotherapy, hematologic malignancy, and HTLV-1 infection. HIV alone is not associated with SHS, however there are rare reports of SHS occurring due to IRIS. The manifestation of intestinal obstruction, worsening respiratory status and gut edema are usually present in severe SHS. It is commonly treated with 14 days of oral ivermectin, however, in patients with severe bowel edema or paralytic ileus, subcutaneous ivermectin may be used as an off-label therapy and is only approved in the veterinary setting. This case highlights the importance of screening or even empirically treating Strongyloides in patients from endemic areas prior to initiating HAART or immunosuppression. We also demonstrate that subcutaneous ivermectin can be used as salvage therapy in patients with SHS.

Disclosures:
Shuhaib Ali, MD1, Kavea Panneerselvam, MD2, Patrick Snyder, MD2, Juan Echavarria, MD2, Onyinye Okonkwo, MD3. P2701 - An Rare Case of Strongyloides Hyperinfection Syndrome as a Manifestation of Immune Reconstituted Inflammatory Syndrome in an HIV-Infected Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1UT Health San Antonio, San Antonio, TX; 2University of Texas Health Science Center at San Antonio, San Antonio, TX; 3UTHSCSA, San Antonio, TX
Introduction: Strongyloides hyperinfection syndrome (SHS) occurs as a result of accelerated autoinfection in patients who have had a sudden change in their immune status. Here, we present a rare case of SHS as a manifestation of immune reconstitution inflammatory syndrome (IRIS) in a patient with HIV, and unconventional treatment with subcutaneous ivermectin.
Case Description/Methods: A 28-year-old male from Honduras was admitted to the hospital with shortness of breath (SOB) and hypoxia. Chest x-ray showed bilateral opacities and lab results confirmed a new diagnosis on HIV. He was discharged on HAART for HIV and corticosteroids for presumed pneumocystis pneumonia. He returned 3 weeks later with worsening SOB, severe abdominal pain, nausea and vomiting. A computed tomography scan showed a partial small bowel obstruction and diffuse wall thickening of the small and large intestine (figure A). HIV-1 PCR viral load decreased from 254,000 copies/mL pre-HAART to 373 copies/mL. Pertinent laboratory tests, including HTLV I/II western blot, Strongyloides IgG serology, AFB cultures, and serial stool ova and parasite screens, yielded negative results. A bronchoscopy confirmed the presence of Strongyloides in the lungs. Colonoscopy showed diffuse wall edema in the colon and ileum (Figure B). Ileal biopsy showed active ileitis with Strongyloides species (Figure C). The patient was treated with ivermectin via nasogastric tube, but concerns of reduced absorption due to gut edema led to a switch to 0.5 ml of 1% ivermectin subcutaneously daily for nine days. His symptoms resolved after 7 days and he was discharged on oral ivermectin to be taken for an additional 14 days.
Discussion: Risk factors for development of SHS include corticosteroid use, chemotherapy, hematologic malignancy, and HTLV-1 infection. HIV alone is not associated with SHS, however there are rare reports of SHS occurring due to IRIS. The manifestation of intestinal obstruction, worsening respiratory status and gut edema are usually present in severe SHS. It is commonly treated with 14 days of oral ivermectin, however, in patients with severe bowel edema or paralytic ileus, subcutaneous ivermectin may be used as an off-label therapy and is only approved in the veterinary setting. This case highlights the importance of screening or even empirically treating Strongyloides in patients from endemic areas prior to initiating HAART or immunosuppression. We also demonstrate that subcutaneous ivermectin can be used as salvage therapy in patients with SHS.

Figure: A. Yellow arrow pointing at thickened ileum
B. Severely congested mucosa in the terminal ileum
C. Active colitis with numerous organisms consistent with Strongyloides species present
B. Severely congested mucosa in the terminal ileum
C. Active colitis with numerous organisms consistent with Strongyloides species present
Disclosures:
Shuhaib Ali indicated no relevant financial relationships.
Kavea Panneerselvam indicated no relevant financial relationships.
Patrick Snyder indicated no relevant financial relationships.
Juan Echavarria indicated no relevant financial relationships.
Onyinye Okonkwo indicated no relevant financial relationships.
Shuhaib Ali, MD1, Kavea Panneerselvam, MD2, Patrick Snyder, MD2, Juan Echavarria, MD2, Onyinye Okonkwo, MD3. P2701 - An Rare Case of Strongyloides Hyperinfection Syndrome as a Manifestation of Immune Reconstituted Inflammatory Syndrome in an HIV-Infected Patient, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
