Monday Poster Session
Category: Stomach
P2764 - Obesity and GERD: An Analysis of the Role of Bariatric Surgery in Reducing the Risk of Adenocarcinoma
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Uma D. Gupta, MD
One Brooklyn Health-Interfaith Medical Center
Brooklyn, NY
Presenting Author(s)
Uma D. Gupta, MD1, Sindhu Pokhriyal, MD2, Manisha Deb, MBBS3, Parinitha Neravanda, MD2, Tahira Fardous, MD4, Govind Dhakal, MD2, Pulok Roy, MD2, Elora Chakraborty, MD5
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Interfaith Medical Center, Brooklyn, NY; 3Sylhet MAG Osmani Medical College and Hospital, Brooklyn, NY; 4Sir Salimullah Medical College and Mitford Hospital, Dhaka, Bangladesh, Brooklyn, NY; 5Dhaka Medical College, Brooklyn, NY
Introduction: Obesity is defined as BMI (Body Mass Index) of 30 kg/m2 or higher, which is a significant contributor to the rise of health issues, including gastroesophageal reflux disease (GERD). In addition, the treatment of GERD, a well-known obesity-related condition, has increased the cost of healthcare in recent years [1].
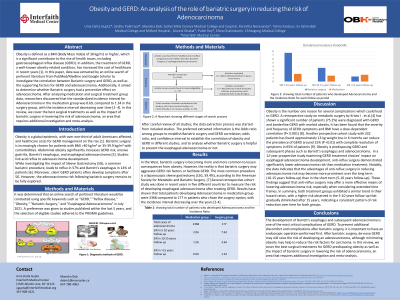
Methods: After an extensive online search from PubMed and Google Scholar with keywords like "GERD," "Bariatric Surgery," and "Esophageal Adenocarcinoma" in July 2021-we decided to do a data extract on two categories: the relation between Bariatric surgery and GERD and Adenocarcinoma prevented by Bariatric surgery or not. Studies within 5 years were preferred, and eligible studies were selected following PRISMA guidelines. Out of 156 studies, only 62 were selected after screening abstracts. We included review articles, cohort studies, case-control studies, and meta-analyses. After carefully reviewing all studies, the data extraction process was started from included studies. The preferred extracted information is the Odds ratio among groups to establish Bariatric surgery and GERD correlation.
Results: The most common procedure is a laparoscopic sleeve gastrectomy (LSG, 59.4%). Borbely et al, found that 66% of preoperative silent GERD develop symptoms after SG (3). However, patients with pre-existing GERD symptoms should undergo endoscopy to rule out any pre-existing Barrett's esophagus as symptoms of GERD may worsen after surgery [4-6].
Discussion: A prospective cohort study was done in recent years in five Nordic Countries to measure the risk of developing esophageal adenocarcinoma after treating GERD .Two groups were selected , with one group choosing to undergo Anti-reflux Surgery while the second group chose the option of medical treatment of either H2 Blocker or PPI inhibitor , both groups had an established GERD before starting the study and were followed for 12 years. Both groups were compared with their correspondent population using standarized Incidence. Interval with 95% CI and Hazards Ratio for cofounders( Age, Sex , DM2 , COPD , obesity and Lost to follow up ) was evaluated. Results have shown that total patients developing Adenocarcinoma in medication group were 2368 compared to 177 in patients who chose the surgery option, with the incidence interval decreasing over the years .
Disclosures:
Uma D. Gupta, MD1, Sindhu Pokhriyal, MD2, Manisha Deb, MBBS3, Parinitha Neravanda, MD2, Tahira Fardous, MD4, Govind Dhakal, MD2, Pulok Roy, MD2, Elora Chakraborty, MD5. P2764 - Obesity and GERD: An Analysis of the Role of Bariatric Surgery in Reducing the Risk of Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Interfaith Medical Center, Brooklyn, NY; 3Sylhet MAG Osmani Medical College and Hospital, Brooklyn, NY; 4Sir Salimullah Medical College and Mitford Hospital, Dhaka, Bangladesh, Brooklyn, NY; 5Dhaka Medical College, Brooklyn, NY
Introduction: Obesity is defined as BMI (Body Mass Index) of 30 kg/m2 or higher, which is a significant contributor to the rise of health issues, including gastroesophageal reflux disease (GERD). In addition, the treatment of GERD, a well-known obesity-related condition, has increased the cost of healthcare in recent years [1].
Methods: After an extensive online search from PubMed and Google Scholar with keywords like "GERD," "Bariatric Surgery," and "Esophageal Adenocarcinoma" in July 2021-we decided to do a data extract on two categories: the relation between Bariatric surgery and GERD and Adenocarcinoma prevented by Bariatric surgery or not. Studies within 5 years were preferred, and eligible studies were selected following PRISMA guidelines. Out of 156 studies, only 62 were selected after screening abstracts. We included review articles, cohort studies, case-control studies, and meta-analyses. After carefully reviewing all studies, the data extraction process was started from included studies. The preferred extracted information is the Odds ratio among groups to establish Bariatric surgery and GERD correlation.
Results: The most common procedure is a laparoscopic sleeve gastrectomy (LSG, 59.4%). Borbely et al, found that 66% of preoperative silent GERD develop symptoms after SG (3). However, patients with pre-existing GERD symptoms should undergo endoscopy to rule out any pre-existing Barrett's esophagus as symptoms of GERD may worsen after surgery [4-6].
Discussion: A prospective cohort study was done in recent years in five Nordic Countries to measure the risk of developing esophageal adenocarcinoma after treating GERD .Two groups were selected , with one group choosing to undergo Anti-reflux Surgery while the second group chose the option of medical treatment of either H2 Blocker or PPI inhibitor , both groups had an established GERD before starting the study and were followed for 12 years. Both groups were compared with their correspondent population using standarized Incidence. Interval with 95% CI and Hazards Ratio for cofounders( Age, Sex , DM2 , COPD , obesity and Lost to follow up ) was evaluated. Results have shown that total patients developing Adenocarcinoma in medication group were 2368 compared to 177 in patients who chose the surgery option, with the incidence interval decreasing over the years .
Disclosures:
Uma Gupta indicated no relevant financial relationships.
Sindhu Pokhriyal indicated no relevant financial relationships.
Manisha Deb indicated no relevant financial relationships.
Parinitha Neravanda indicated no relevant financial relationships.
Tahira Fardous indicated no relevant financial relationships.
Govind Dhakal indicated no relevant financial relationships.
Pulok Roy indicated no relevant financial relationships.
Elora Chakraborty indicated no relevant financial relationships.
Uma D. Gupta, MD1, Sindhu Pokhriyal, MD2, Manisha Deb, MBBS3, Parinitha Neravanda, MD2, Tahira Fardous, MD4, Govind Dhakal, MD2, Pulok Roy, MD2, Elora Chakraborty, MD5. P2764 - Obesity and GERD: An Analysis of the Role of Bariatric Surgery in Reducing the Risk of Adenocarcinoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
