Monday Poster Session
Category: Stomach
P2776 - An Unusual Cause of Abdominal Bloating
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- HR
Harini Rathinamanickam, MD
SIU School of Medicine
Springfield, IL
Presenting Author(s)
Harini Rathinamanickam, MD
SIU School of Medicine, Springfield, IL
Introduction: Eosinophilic Gastro Intestinal Disorders (EGID) are eosinophilic infiltrative disorders of the gastrointestinal (GI) tract. EGID includes Eosinophilic esophagitis (EoE), Eosinophilic Gastritis (EG), Eosinophilic gastroenteritis (EGE) and Eosinophilic Colitis ( EC). Non-EoE EGIDs are rare with a prevalence of 5.3/10000. Here we report a rare case of EG in an elderly man presenting with abdominal bloating.
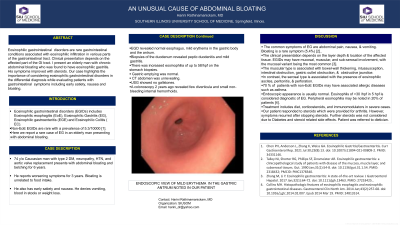
Case Description/Methods: 74 y/o Caucasian man with type 2 DM, neuropathy, HTN, and aortic valve replacement presents with abdominal bloating and belching for 6 years. He reports worsening symptoms for 3 years. Bloating is unrelated to food intake. He also has early satiety and nausea. He denies vomiting, blood in stools or weight loss. EGD revealed normal esophagus, mild erythema in the gastric body and the antrum. Biopsies of the duodenum revealed peptic duodenitis and mild gastritis. There was increased eosinophilia of up to 58/hpf on the stomach biopsies. Gastric emptying was normal. CT abdomen was unrevealing. USG showed no gallstones. A colonoscopy 2 years ago revealed few diverticula and small non-bleeding internal hemorrhoids.
Discussion: The common symptoms of EG are abdominal pain, nausea, and vomiting. Bloating was a rare symptom (5.4%) in a study. The clinical presentation depends on the layer depth and location of the affected tissue. EGs may have mucosal, muscular, and sub-serosal involvement, with the mucosal variant being the most common. The muscular type is associated with bowel-wall thickening, intussusception, intestinal obstruction, gastric outlet obstruction, and obstructive jaundice. In contrast, the serosal type is associated with the presence of eosinophilic ascites, peritonitis, and perforation. 70 % of patients with non-EoE EGIDs may have associated allergic diseases such as asthma.
The most common EGD appearance is normal. Eosinophils of >20 /hpf is considered diagnostic. Peripheral eosinophilia may be noted in 20% of patients. Treatment is by diet, corticosteroids, and immunomodulators in severe cases. Our patient responded to steroids which were provided for arthritis. However, symptoms recurred after stopping steroids.
Our case highlights the importance of considering EG in the differential diagnosis while evaluating patients with upper gastrointestinal symptoms such as bloating.

Disclosures:
Harini Rathinamanickam, MD. P2776 - An Unusual Cause of Abdominal Bloating, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
SIU School of Medicine, Springfield, IL
Introduction: Eosinophilic Gastro Intestinal Disorders (EGID) are eosinophilic infiltrative disorders of the gastrointestinal (GI) tract. EGID includes Eosinophilic esophagitis (EoE), Eosinophilic Gastritis (EG), Eosinophilic gastroenteritis (EGE) and Eosinophilic Colitis ( EC). Non-EoE EGIDs are rare with a prevalence of 5.3/10000. Here we report a rare case of EG in an elderly man presenting with abdominal bloating.
Case Description/Methods: 74 y/o Caucasian man with type 2 DM, neuropathy, HTN, and aortic valve replacement presents with abdominal bloating and belching for 6 years. He reports worsening symptoms for 3 years. Bloating is unrelated to food intake. He also has early satiety and nausea. He denies vomiting, blood in stools or weight loss. EGD revealed normal esophagus, mild erythema in the gastric body and the antrum. Biopsies of the duodenum revealed peptic duodenitis and mild gastritis. There was increased eosinophilia of up to 58/hpf on the stomach biopsies. Gastric emptying was normal. CT abdomen was unrevealing. USG showed no gallstones. A colonoscopy 2 years ago revealed few diverticula and small non-bleeding internal hemorrhoids.
Discussion: The common symptoms of EG are abdominal pain, nausea, and vomiting. Bloating was a rare symptom (5.4%) in a study. The clinical presentation depends on the layer depth and location of the affected tissue. EGs may have mucosal, muscular, and sub-serosal involvement, with the mucosal variant being the most common. The muscular type is associated with bowel-wall thickening, intussusception, intestinal obstruction, gastric outlet obstruction, and obstructive jaundice. In contrast, the serosal type is associated with the presence of eosinophilic ascites, peritonitis, and perforation. 70 % of patients with non-EoE EGIDs may have associated allergic diseases such as asthma.
The most common EGD appearance is normal. Eosinophils of >20 /hpf is considered diagnostic. Peripheral eosinophilia may be noted in 20% of patients. Treatment is by diet, corticosteroids, and immunomodulators in severe cases. Our patient responded to steroids which were provided for arthritis. However, symptoms recurred after stopping steroids.
Our case highlights the importance of considering EG in the differential diagnosis while evaluating patients with upper gastrointestinal symptoms such as bloating.

Figure: Endoscopic view of mild erythema in the gastric antrum noted in our patient.
Disclosures:
Harini Rathinamanickam indicated no relevant financial relationships.
Harini Rathinamanickam, MD. P2776 - An Unusual Cause of Abdominal Bloating, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
