Monday Poster Session
Category: Stomach
P2790 - Septic Gastric Perforation Resolves Without Surgical Intervention: A Case Report
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- DP
David Putt, DO, MBA
Ascension Providence/MSUCHM Program
Southfield, Michigan
Presenting Author(s)
David Putt, DO, MBA1, George Felemegos, MD1, Saif Affas, MD2
1Ascension Providence/MSUCHM Program, Southfield, MI; 2Ascension Providence Hospital, Troy, MI
Introduction: Patients with evidence of gastrointestinal perforation and clinical sepsis benefit from immediate surgery. Definitive surgical treatment should be done at the earliest possible time. Herein, we report a case of septic gastric perforation that resolved with conservative non-operative management.
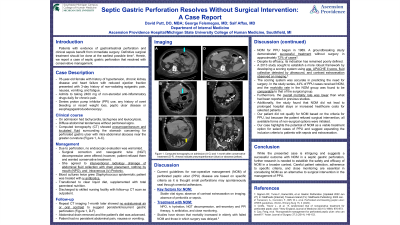
Case Description/Methods: A 76 year old female with a history of chronic kidney disease and heart failure presented for epigastric pain, nausea, vomiting, and fatigue. She had been taking 2400 mg of NSAIDs daily for chronic pain. She denied PPI use as well as any overt bleeding. No history of PUD or EGD. On admission the patient was tachycardic, tachypneic, and had leukocytosis. Physical exam showed no peritoneal signs but abdominal tenderness. CT showed pneumoperitoneum and loculated fluid collections surrounding the stomach. Surgical correction was offered to the patient, however, the patient refused surgery and nasogastric tube placement. Blood cultures grew Staphylococcus Epidermidis. Patient was treated with antibiotics, IR drainage of the fluid collection with drain placement, NPO, and IV Protonix. Patient was nonadherent with NPO order. The patient understood the risks of infection at the time of discharge and still chose conservative medical management. She was discharged to a skilled nursing facility with IV antibiotics, abdominal drain in place, TPN, CLD, and follow up scan as an outpatient. One month later, imaging showed no extraluminal air or oral contrast to suggest persistent/recurrent gastric perforation. The abdominal drain was removed and the patient was cleared for regular diet and had no further symptoms.
Discussion: Current guidelines indicate non-operative management (NOM) of perforated peptic ulcer disease in select cases with specific criteria including stable vital signs, absence of contrast extravasation on imaging, and the absence of peritonitis or sepsis. All of these criteria should have excluded our patient from receiving conservative management and indicated a higher risk of complication if surgical intervention was not completed. However, despite lack of surgical intervention, repeat imaging proved closure of the perforation indicating a successful outcome with NOM. These findings highlight the potential of NOM as a viable treatment option for selected cases of gastric perforation, and suggest expanding the inclusion criteria to patients with sepsis and extravasation on imaging. Further research is needed to establish the safety and efficacy of NOM in a broader context.
Disclosures:
David Putt, DO, MBA1, George Felemegos, MD1, Saif Affas, MD2. P2790 - Septic Gastric Perforation Resolves Without Surgical Intervention: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Ascension Providence/MSUCHM Program, Southfield, MI; 2Ascension Providence Hospital, Troy, MI
Introduction: Patients with evidence of gastrointestinal perforation and clinical sepsis benefit from immediate surgery. Definitive surgical treatment should be done at the earliest possible time. Herein, we report a case of septic gastric perforation that resolved with conservative non-operative management.
Case Description/Methods: A 76 year old female with a history of chronic kidney disease and heart failure presented for epigastric pain, nausea, vomiting, and fatigue. She had been taking 2400 mg of NSAIDs daily for chronic pain. She denied PPI use as well as any overt bleeding. No history of PUD or EGD. On admission the patient was tachycardic, tachypneic, and had leukocytosis. Physical exam showed no peritoneal signs but abdominal tenderness. CT showed pneumoperitoneum and loculated fluid collections surrounding the stomach. Surgical correction was offered to the patient, however, the patient refused surgery and nasogastric tube placement. Blood cultures grew Staphylococcus Epidermidis. Patient was treated with antibiotics, IR drainage of the fluid collection with drain placement, NPO, and IV Protonix. Patient was nonadherent with NPO order. The patient understood the risks of infection at the time of discharge and still chose conservative medical management. She was discharged to a skilled nursing facility with IV antibiotics, abdominal drain in place, TPN, CLD, and follow up scan as an outpatient. One month later, imaging showed no extraluminal air or oral contrast to suggest persistent/recurrent gastric perforation. The abdominal drain was removed and the patient was cleared for regular diet and had no further symptoms.
Discussion: Current guidelines indicate non-operative management (NOM) of perforated peptic ulcer disease in select cases with specific criteria including stable vital signs, absence of contrast extravasation on imaging, and the absence of peritonitis or sepsis. All of these criteria should have excluded our patient from receiving conservative management and indicated a higher risk of complication if surgical intervention was not completed. However, despite lack of surgical intervention, repeat imaging proved closure of the perforation indicating a successful outcome with NOM. These findings highlight the potential of NOM as a viable treatment option for selected cases of gastric perforation, and suggest expanding the inclusion criteria to patients with sepsis and extravasation on imaging. Further research is needed to establish the safety and efficacy of NOM in a broader context.
Disclosures:
David Putt indicated no relevant financial relationships.
George Felemegos indicated no relevant financial relationships.
Saif Affas indicated no relevant financial relationships.
David Putt, DO, MBA1, George Felemegos, MD1, Saif Affas, MD2. P2790 - Septic Gastric Perforation Resolves Without Surgical Intervention: A Case Report, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
