Monday Poster Session
Category: Stomach
P2816 - Cyclic Vomiting Syndrome Presenting as Gastric Sarcoidosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Stephanie Ibarra, MD
East Carolina University
Greenville, NC
Presenting Author(s)
Husam El Sharu, MD, Stephanie Ibarra, MD, Zarak Khan, MD, Danielle Hoo-Fatt, MD
East Carolina University, Greenville, NC
Introduction: Sarcoidosis is a multisystemic noncaseating granulomatous disease that primarily affects African American females. Sarcoidosis with GI affection is very rare, presenting in 0.1% to 1.6% of the total cases, with the most common site of involvement being the gastric antrum resulting in broad symptoms and a difficult diagnosis
Case Description/Methods: A 46-year-old African American female with a history of type DM, gallstone pancreatitis, and gastroparesis presented with 30 years of episodic epigastric abdominal pain, intractable nausea and vomiting, and diarrhea. She was initially diagnosed with cyclic vomiting syndrome and had tried various antiemetic regimens and pyloric Botox injection with no relief. She has a family history of sarcoidosis in her brother. The patient smokes tobacco but denies the use of other recreational drugs. Physical exam was remarkable for severe diffuse abdominal tenderness. Labs showed normal LFTs, lipase, and cortisol. Infectious workups for HIV, viral hepatitis, clostridium difficile, and stool parasites were negative. The patient had multiple upper and lower endoscopies, which showed antral erythema with unexplained antral gastritis. CT of the abdomen and pelvis showed mildly thickened right and transverse colon and mild retroperitoneal lymphadenopathy in the celiac axis and porta hepatis. This was treated with prolonged courses of different PPIs with no improvement. Due to the persistence of symptoms, the patient underwent an EGD with a EUS, which showed a normal esophagus, stomach, and duodenum endoscopically. EUS findings were consistent with few lymph nodes visualized in the peri-gastric and peri-duodenal region, with the largest being 15mm. Cytology and antral gastric biopsy showed noncaseating granulomas with negative Gomori methenamine silver and AFB stains. CT of the chest showed right upper lobe ground glass opacity with no hilar or mediastinal lymphadenopathy. The patient was started on prednisone with significant improvement in symptoms. On follow-up, she did not have any episodes of nausea or vomiting.
Discussion: This case illustrates an example of gastrointestinal sarcoidosis, a scarce variant of noncaseating granulomatous disease, with a nonspecific clinical picture. Our patient had no indication of intrapulmonary involvement, which made the diagnosis even more difficult. More attention is required to include sarcoidosis as a plausible etiological factor in gastrointestinal disease.

Disclosures:
Husam El Sharu, MD, Stephanie Ibarra, MD, Zarak Khan, MD, Danielle Hoo-Fatt, MD. P2816 - Cyclic Vomiting Syndrome Presenting as Gastric Sarcoidosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
East Carolina University, Greenville, NC
Introduction: Sarcoidosis is a multisystemic noncaseating granulomatous disease that primarily affects African American females. Sarcoidosis with GI affection is very rare, presenting in 0.1% to 1.6% of the total cases, with the most common site of involvement being the gastric antrum resulting in broad symptoms and a difficult diagnosis
Case Description/Methods: A 46-year-old African American female with a history of type DM, gallstone pancreatitis, and gastroparesis presented with 30 years of episodic epigastric abdominal pain, intractable nausea and vomiting, and diarrhea. She was initially diagnosed with cyclic vomiting syndrome and had tried various antiemetic regimens and pyloric Botox injection with no relief. She has a family history of sarcoidosis in her brother. The patient smokes tobacco but denies the use of other recreational drugs. Physical exam was remarkable for severe diffuse abdominal tenderness. Labs showed normal LFTs, lipase, and cortisol. Infectious workups for HIV, viral hepatitis, clostridium difficile, and stool parasites were negative. The patient had multiple upper and lower endoscopies, which showed antral erythema with unexplained antral gastritis. CT of the abdomen and pelvis showed mildly thickened right and transverse colon and mild retroperitoneal lymphadenopathy in the celiac axis and porta hepatis. This was treated with prolonged courses of different PPIs with no improvement. Due to the persistence of symptoms, the patient underwent an EGD with a EUS, which showed a normal esophagus, stomach, and duodenum endoscopically. EUS findings were consistent with few lymph nodes visualized in the peri-gastric and peri-duodenal region, with the largest being 15mm. Cytology and antral gastric biopsy showed noncaseating granulomas with negative Gomori methenamine silver and AFB stains. CT of the chest showed right upper lobe ground glass opacity with no hilar or mediastinal lymphadenopathy. The patient was started on prednisone with significant improvement in symptoms. On follow-up, she did not have any episodes of nausea or vomiting.
Discussion: This case illustrates an example of gastrointestinal sarcoidosis, a scarce variant of noncaseating granulomatous disease, with a nonspecific clinical picture. Our patient had no indication of intrapulmonary involvement, which made the diagnosis even more difficult. More attention is required to include sarcoidosis as a plausible etiological factor in gastrointestinal disease.

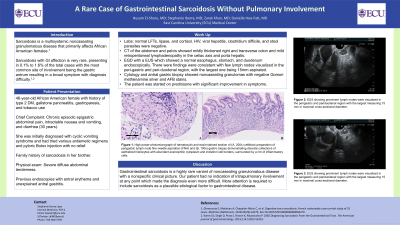
Figure: EUS showing prominent lymph nodes were visualized in the perigastric and periduodenal region, with the largest measuring 15 mm in maximal cross-sectional diameter.
High-power photomicrograph of hematoxylin and eosin-stained section of (A, 200x) cellblock preparation of a perigastric lymph node fine needle aspiration (FNA) and (B, 100x) gastric biopsy demonstrating discrete collections of epithelioid histiocytes with abundant eosinophilic cytoplasm and indistinct cell borders, surrounded by a rim of inflammatory cells.
High-power photomicrograph of hematoxylin and eosin-stained section of (A, 200x) cellblock preparation of a perigastric lymph node fine needle aspiration (FNA) and (B, 100x) gastric biopsy demonstrating discrete collections of epithelioid histiocytes with abundant eosinophilic cytoplasm and indistinct cell borders, surrounded by a rim of inflammatory cells.
Disclosures:
Husam El Sharu indicated no relevant financial relationships.
Stephanie Ibarra indicated no relevant financial relationships.
Zarak Khan indicated no relevant financial relationships.
Danielle Hoo-Fatt indicated no relevant financial relationships.
Husam El Sharu, MD, Stephanie Ibarra, MD, Zarak Khan, MD, Danielle Hoo-Fatt, MD. P2816 - Cyclic Vomiting Syndrome Presenting as Gastric Sarcoidosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
