Monday Poster Session
Category: Stomach
P2818 - Two Cases of Ischemic Gastritis Secondary to Septic Emboli
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Tyler M. Selig, MD
Warren Alpert Medical School of Brown University/Lifespan
Providence, RI
Presenting Author(s)
Tyler M.. Selig, MD1, Yousef Elfanagely, MD2, William Park, MD3, Kanhai Farrakhan, MD2, Colleen R. Kelly, MD, FACG4, May Min, MD5
1Warren Alpert Medical School of Brown University/Lifespan, Providence, RI; 2Warren Alpert Medical School of Brown University, Providence, RI; 3Brown University, Providence, RI; 4Alpert School of Medicine of Brown University, Providence, RI; 5Warren Alpert Medical School/Lifespan Physician Group, Providence, RI
Introduction: We present two cases of ischemic gastritis, which is a rare cause of gastric mucosal injury given the robust collateral blood supply to the stomach. Both patients had diffuse septic emboli from infectious endocarditis without an IVDU history. Due to its >70% mortality rate, ischemic gastritis must be on the differential when patients present with endocarditis.
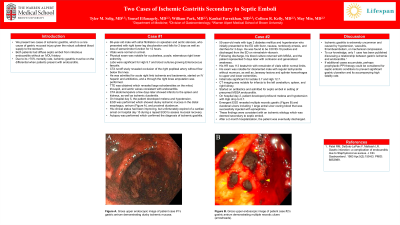
Case Description/Methods: The 1st case is a 69-year-old male with AF on apixaban who presented with right leg discoloration and sensorimotor loss for 2 days. Vitals were normal and physical exam was notable for a pulseless right lower extremity. Labs were significant for Hgb 9.7 g/dL and blood cultures growing E. faecalis. He was started antibiotics and a through the right knee amputation was performed. TTE demonstrated large echodensities on the mitral, tricuspid, and aortic valves consistent with endocarditis. CTA showed infarcts to the spleen and kidneys, as well as ischemic duodenitis. On hospital day 5, the patient developed melena and hypotension. EGD was performed which showed dusky ischemic mucosa in the distal esophagus, gastric antrum (Figure A), and proximal duodenum. He later expired of a cardiac arrest and autopsy confirmed a diagnosis of ischemic gastritis.
The 2nd case is a 55-year-old male with T2DM who presented with confusion and weakness for 3 days. His HR was 113 beats/min with otherwise normal vitals. His exam was notable for Janeway lesions and splinter hemorrhages. Initial labs significant for Hgb 12.7 g/dL and blood cultures growing MSSA. CT imaging was notable for infarcts to the left cerebellum, spleen, and right kidney. TTE revealed new mitral regurgitation without identifiable vegetation. Patient was started on antibiotics for septic emboli in setting of presumed MSSA endocarditis. On hospital day 2, patient developed melena and hypotension with Hgb drop to 8.7 g/dL. An emergent EGD revealed multiple necrotic gastric (Figure B) and duodenal ulcers, which were consistent with an ischemic etiology deemed secondary to septic emboli. He was discharged after 2 months.
Discussion: Ischemic gastritis is extremely uncommon and caused by hypotension, vasculitis, thromboembolism, or mechanical compression. To our knowledge, only 1 case has been published discussing a relationship between gastric ischemia and endocarditis. If additional cases accumulate, perhaps prophylactic PPI therapy could be considered for septic embolic conditions to prevent significant gastric ulceration and its accompanying high fatality rate.

Disclosures:
Tyler M.. Selig, MD1, Yousef Elfanagely, MD2, William Park, MD3, Kanhai Farrakhan, MD2, Colleen R. Kelly, MD, FACG4, May Min, MD5. P2818 - Two Cases of Ischemic Gastritis Secondary to Septic Emboli, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Warren Alpert Medical School of Brown University/Lifespan, Providence, RI; 2Warren Alpert Medical School of Brown University, Providence, RI; 3Brown University, Providence, RI; 4Alpert School of Medicine of Brown University, Providence, RI; 5Warren Alpert Medical School/Lifespan Physician Group, Providence, RI
Introduction: We present two cases of ischemic gastritis, which is a rare cause of gastric mucosal injury given the robust collateral blood supply to the stomach. Both patients had diffuse septic emboli from infectious endocarditis without an IVDU history. Due to its >70% mortality rate, ischemic gastritis must be on the differential when patients present with endocarditis.
Case Description/Methods: The 1st case is a 69-year-old male with AF on apixaban who presented with right leg discoloration and sensorimotor loss for 2 days. Vitals were normal and physical exam was notable for a pulseless right lower extremity. Labs were significant for Hgb 9.7 g/dL and blood cultures growing E. faecalis. He was started antibiotics and a through the right knee amputation was performed. TTE demonstrated large echodensities on the mitral, tricuspid, and aortic valves consistent with endocarditis. CTA showed infarcts to the spleen and kidneys, as well as ischemic duodenitis. On hospital day 5, the patient developed melena and hypotension. EGD was performed which showed dusky ischemic mucosa in the distal esophagus, gastric antrum (Figure A), and proximal duodenum. He later expired of a cardiac arrest and autopsy confirmed a diagnosis of ischemic gastritis.
The 2nd case is a 55-year-old male with T2DM who presented with confusion and weakness for 3 days. His HR was 113 beats/min with otherwise normal vitals. His exam was notable for Janeway lesions and splinter hemorrhages. Initial labs significant for Hgb 12.7 g/dL and blood cultures growing MSSA. CT imaging was notable for infarcts to the left cerebellum, spleen, and right kidney. TTE revealed new mitral regurgitation without identifiable vegetation. Patient was started on antibiotics for septic emboli in setting of presumed MSSA endocarditis. On hospital day 2, patient developed melena and hypotension with Hgb drop to 8.7 g/dL. An emergent EGD revealed multiple necrotic gastric (Figure B) and duodenal ulcers, which were consistent with an ischemic etiology deemed secondary to septic emboli. He was discharged after 2 months.
Discussion: Ischemic gastritis is extremely uncommon and caused by hypotension, vasculitis, thromboembolism, or mechanical compression. To our knowledge, only 1 case has been published discussing a relationship between gastric ischemia and endocarditis. If additional cases accumulate, perhaps prophylactic PPI therapy could be considered for septic embolic conditions to prevent significant gastric ulceration and its accompanying high fatality rate.

Figure: Figure A. Gross upper endoscopic image of patient case #1’s gastric antrum demonstrating dusky ischemic mucosa.
Figure B. Gross upper endoscopic image of patient case #2’s gastric antrum demonstrating multiple necrotic ulcers (arrowheads).
Figure B. Gross upper endoscopic image of patient case #2’s gastric antrum demonstrating multiple necrotic ulcers (arrowheads).
Disclosures:
Tyler Selig indicated no relevant financial relationships.
Yousef Elfanagely indicated no relevant financial relationships.
William Park indicated no relevant financial relationships.
Kanhai Farrakhan indicated no relevant financial relationships.
Colleen Kelly: Sebela Pharmaceuticals – Consultant.
May Min indicated no relevant financial relationships.
Tyler M.. Selig, MD1, Yousef Elfanagely, MD2, William Park, MD3, Kanhai Farrakhan, MD2, Colleen R. Kelly, MD, FACG4, May Min, MD5. P2818 - Two Cases of Ischemic Gastritis Secondary to Septic Emboli, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
