Monday Poster Session
Category: Stomach
P2820 - Perforated Gastric Ulcer Complicated by Peritonitis and Pelvic Abscesses in a Patient with Diabetic Ketoacidosis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
.jpg)
Sarah Huang, MD
New York Presbyterian Brooklyn Methodist Hospital
Brooklyn, New York
Presenting Author(s)
Sarah Huang, MD1, Harsh Patel, MD2, Navim Mobin, MD1, Meghaben Kothari, MD2
1New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist, Brooklyn, NY
Introduction: The incidence of peptic ulcer disease (PUD) is 0.1 - 0.3% annually and affects 5-10% of the general population. It is commonly caused by H. pylori and NSAID use, with a potential to perforate, leading to peritonitis. Perforated peptic ulcers have a high mortality rate of 40-60% with improved outcome after antibiotics and surgical intervention.
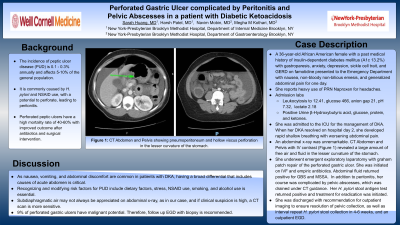
Case Description/Methods: A 36-year-old African American female with a past medical history of insulin-dependent diabetes mellitus (A1c 13.2%) with gastroparesis, anxiety, depression, sickle cell trait, and GERD on famotidine presented to the Emergency Department with nausea, non-bloody non-bilious emesis, and generalized abdominal pain for one day. She reports heavy use of naproxen as needed for headaches. Admission labs were remarkable for leukocytosis to 12.41, glucose 466, anion gap 21, pH 7.32, lactate 2.18, with positive urine β-Hydroxybutyric acid, glucose, protein, and ketones. She was admitted to the ICU for the management of DKA. When her DKA resolved on hospital day 2, she developed rapid shallow breathing with worsening abdominal pain. An abdominal x-ray was unremarkable. CT Abdomen and Pelvis with IV contrast (Figure 1) revealed a large amount of free air and fluid in the lesser curvature of the stomach. She underwent emergent exploratory laparotomy with graham patch repair of the perforated gastric ulcer. She was initiated on intravenous fluids and empiric antibiotics. Abdominal fluid returned positive for GBS and MSSA. In addition to peritonitis, her course was complicated by pelvic abscesses, which was drained under CT guidance. Her H. pylori stool antigen test returned positive and treatment for eradication was initiated. She was discharged with recommendation for outpatient imaging to ensure resolution of pelvic collection, as well as a repeat H. pylori stool collection in 4-6 weeks, and an outpatient EGD.
Discussion: As nausea, vomiting, and abdominal discomfort are common in patients with DKA, having a broad differential that includes causes of acute abdomen is critical. Recognizing and modifying risk factors for PUD include dietary factors, stress, NSAID use, smoking, and alcohol use is essential. Subdiaphragmatic air may not always be appreciated on abdominal x-ray, as in our case, and if clinical suspicion is high, a CT scan is more sensitive. Nine percent of perforated gastric ulcers have malignant potential. Therefore, follow up EGD with biopsy is recommended.

Disclosures:
Sarah Huang, MD1, Harsh Patel, MD2, Navim Mobin, MD1, Meghaben Kothari, MD2. P2820 - Perforated Gastric Ulcer Complicated by Peritonitis and Pelvic Abscesses in a Patient with Diabetic Ketoacidosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 2New York Presbyterian Brooklyn Methodist, Brooklyn, NY
Introduction: The incidence of peptic ulcer disease (PUD) is 0.1 - 0.3% annually and affects 5-10% of the general population. It is commonly caused by H. pylori and NSAID use, with a potential to perforate, leading to peritonitis. Perforated peptic ulcers have a high mortality rate of 40-60% with improved outcome after antibiotics and surgical intervention.
Case Description/Methods: A 36-year-old African American female with a past medical history of insulin-dependent diabetes mellitus (A1c 13.2%) with gastroparesis, anxiety, depression, sickle cell trait, and GERD on famotidine presented to the Emergency Department with nausea, non-bloody non-bilious emesis, and generalized abdominal pain for one day. She reports heavy use of naproxen as needed for headaches. Admission labs were remarkable for leukocytosis to 12.41, glucose 466, anion gap 21, pH 7.32, lactate 2.18, with positive urine β-Hydroxybutyric acid, glucose, protein, and ketones. She was admitted to the ICU for the management of DKA. When her DKA resolved on hospital day 2, she developed rapid shallow breathing with worsening abdominal pain. An abdominal x-ray was unremarkable. CT Abdomen and Pelvis with IV contrast (Figure 1) revealed a large amount of free air and fluid in the lesser curvature of the stomach. She underwent emergent exploratory laparotomy with graham patch repair of the perforated gastric ulcer. She was initiated on intravenous fluids and empiric antibiotics. Abdominal fluid returned positive for GBS and MSSA. In addition to peritonitis, her course was complicated by pelvic abscesses, which was drained under CT guidance. Her H. pylori stool antigen test returned positive and treatment for eradication was initiated. She was discharged with recommendation for outpatient imaging to ensure resolution of pelvic collection, as well as a repeat H. pylori stool collection in 4-6 weeks, and an outpatient EGD.
Discussion: As nausea, vomiting, and abdominal discomfort are common in patients with DKA, having a broad differential that includes causes of acute abdomen is critical. Recognizing and modifying risk factors for PUD include dietary factors, stress, NSAID use, smoking, and alcohol use is essential. Subdiaphragmatic air may not always be appreciated on abdominal x-ray, as in our case, and if clinical suspicion is high, a CT scan is more sensitive. Nine percent of perforated gastric ulcers have malignant potential. Therefore, follow up EGD with biopsy is recommended.

Figure: Figure 1: CT Abdomen and Pelvis showing pneumoperitoneum and hollow viscus perforation in the lesser curvature of the stomach.
Disclosures:
Sarah Huang indicated no relevant financial relationships.
Harsh Patel indicated no relevant financial relationships.
Navim Mobin indicated no relevant financial relationships.
Meghaben Kothari indicated no relevant financial relationships.
Sarah Huang, MD1, Harsh Patel, MD2, Navim Mobin, MD1, Meghaben Kothari, MD2. P2820 - Perforated Gastric Ulcer Complicated by Peritonitis and Pelvic Abscesses in a Patient with Diabetic Ketoacidosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
