Monday Poster Session
Category: Stomach
P2752 - Study Design Considerations for Thoracic Neuromodulation in Diabetic Gastroparesis
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
- DS
Dhanush Shimoga, MBBS
Medical College of Georgia at Augusta University
Augusta, GA
Presenting Author(s)
Award: Presidential Poster Award
Dhanush Shimoga, MBBS1, Andrew Bolender, 2, Roberta Sclocco, PhD2, Tennekoon B. Karunaratne, MD, PhD3, Braden Kuo, MD2, Amol Sharma, MD, MS, FACG1
1Medical College of Georgia at Augusta University, Augusta, GA; 2Massachusetts General Hospital, Boston, MA; 3Augusta University, Augusta, GA
Introduction: Diabetic gastroparesis (DGp) is a significant condition that lacks effective treatment. We aim to assess study design considerations pooled from our experience in a phase 1a study and our ongoing phase 1b RCT.
Methods: Adult DGp subjects meeting inclusion/exclusion criteria signed an informed consent (IRB 1623939 &1870454) and were enrolled into a phase 1a or 1b study (NCT 04706832 & 05273788). Studies were and are being performed at MCG and MGH. Subjects had moderate-severe DGp symptoms defined as ANMS GCSI-DD total score (7-day average) ≥2.0. Enrolled subjects had neuromodulation with a repetitive coil resting on the back over bilateral T7 spinal nerves in the supine position, delivering 1200 repetitive magnetic stimulation for 5 days. During the phase 1a study, optimal treatment parameters and location were determined. In the ongoing phase 1b, enrolled subjects are randomized to sham, 1-Hz and 10-Hz treatment arms following an optimized protocol. Primary endpoint is ≥30% decrease of total ANMS GCSI-DD score from baseline. Diaries are maintained during baseline week and for 1 month after start of treatment. Multiple secondary measures are being evaluated including mechanistic fMRI studies.
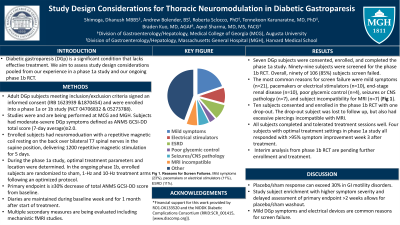
Results: Seven DGp subjects were consented, enrolled, and completed the phase 1a study. Ninety-nine subjects were screened for the phase 1b RCT. Overall, ninety of 106 (85%) subjects screen failed. The most common reasons for screen failure were mild symptoms (n=21), pacemakers or electrical stimulators (n=10), end-stage renal disease (n=10), poor glycemic control (n=4), seizures or CNS pathology (n=7), and subject incompatibility for MRI (n=7) (Fig 1). Ten subjects consented and enrolled in the phase 1b RCT with one drop-out. The drop-out subject was lost to follow up, but also had excessive piercings incompatible with MRI. All subjects completed and tolerated treatment sessions well. Four subjects with optimal treatment settings in phase 1a study all responded with >95% symptom improvement week 3 after treatment. Interim analysis from phase 1b RCT are pending further enrollment.
Discussion: Placebo/sham response can exceed 30% in GI motility disorders. Study subject enrichment with higher symptom severity and delayed assessment of primary endpoint >2 weeks allows for placebo/sham washout. Mild DGp symptoms and electrical devices are common reasons for screen failure.
Acknowledgement: Supported by DiaComp DK076169 & DK115255 and R01 DK133520.

Disclosures:
Dhanush Shimoga, MBBS1, Andrew Bolender, 2, Roberta Sclocco, PhD2, Tennekoon B. Karunaratne, MD, PhD3, Braden Kuo, MD2, Amol Sharma, MD, MS, FACG1. P2752 - Study Design Considerations for Thoracic Neuromodulation in Diabetic Gastroparesis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Dhanush Shimoga, MBBS1, Andrew Bolender, 2, Roberta Sclocco, PhD2, Tennekoon B. Karunaratne, MD, PhD3, Braden Kuo, MD2, Amol Sharma, MD, MS, FACG1
1Medical College of Georgia at Augusta University, Augusta, GA; 2Massachusetts General Hospital, Boston, MA; 3Augusta University, Augusta, GA
Introduction: Diabetic gastroparesis (DGp) is a significant condition that lacks effective treatment. We aim to assess study design considerations pooled from our experience in a phase 1a study and our ongoing phase 1b RCT.
Methods: Adult DGp subjects meeting inclusion/exclusion criteria signed an informed consent (IRB 1623939 &1870454) and were enrolled into a phase 1a or 1b study (NCT 04706832 & 05273788). Studies were and are being performed at MCG and MGH. Subjects had moderate-severe DGp symptoms defined as ANMS GCSI-DD total score (7-day average) ≥2.0. Enrolled subjects had neuromodulation with a repetitive coil resting on the back over bilateral T7 spinal nerves in the supine position, delivering 1200 repetitive magnetic stimulation for 5 days. During the phase 1a study, optimal treatment parameters and location were determined. In the ongoing phase 1b, enrolled subjects are randomized to sham, 1-Hz and 10-Hz treatment arms following an optimized protocol. Primary endpoint is ≥30% decrease of total ANMS GCSI-DD score from baseline. Diaries are maintained during baseline week and for 1 month after start of treatment. Multiple secondary measures are being evaluated including mechanistic fMRI studies.
Results: Seven DGp subjects were consented, enrolled, and completed the phase 1a study. Ninety-nine subjects were screened for the phase 1b RCT. Overall, ninety of 106 (85%) subjects screen failed. The most common reasons for screen failure were mild symptoms (n=21), pacemakers or electrical stimulators (n=10), end-stage renal disease (n=10), poor glycemic control (n=4), seizures or CNS pathology (n=7), and subject incompatibility for MRI (n=7) (Fig 1). Ten subjects consented and enrolled in the phase 1b RCT with one drop-out. The drop-out subject was lost to follow up, but also had excessive piercings incompatible with MRI. All subjects completed and tolerated treatment sessions well. Four subjects with optimal treatment settings in phase 1a study all responded with >95% symptom improvement week 3 after treatment. Interim analysis from phase 1b RCT are pending further enrollment.
Discussion: Placebo/sham response can exceed 30% in GI motility disorders. Study subject enrichment with higher symptom severity and delayed assessment of primary endpoint >2 weeks allows for placebo/sham washout. Mild DGp symptoms and electrical devices are common reasons for screen failure.
Acknowledgement: Supported by DiaComp DK076169 & DK115255 and R01 DK133520.

Figure: Fig 1. Pie chart showing reasons for DGp subject screen fails for across both phase 1a proof-of-concept study and phase 1b RCT.
Disclosures:
Dhanush Shimoga indicated no relevant financial relationships.
Andrew Bolender indicated no relevant financial relationships.
Roberta Sclocco indicated no relevant financial relationships.
Tennekoon Karunaratne indicated no relevant financial relationships.
Braden Kuo indicated no relevant financial relationships.
Amol Sharma indicated no relevant financial relationships.
Dhanush Shimoga, MBBS1, Andrew Bolender, 2, Roberta Sclocco, PhD2, Tennekoon B. Karunaratne, MD, PhD3, Braden Kuo, MD2, Amol Sharma, MD, MS, FACG1. P2752 - Study Design Considerations for Thoracic Neuromodulation in Diabetic Gastroparesis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

