Monday Poster Session
Category: Stomach
P2755 - Race, Preferred Language, and Treatment Regimen Predict Helicobacter pylori Eradication Success in the BOSTON-HP Cohort
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Christina Lee, MD
Beth Israel Deaconess Medical Center, Harvard Medical School
Boston, MA
Presenting Author(s)
Christina Lee, MD1, Marco A. Noriega, MD2, Joseph D. Feuerstein, MD2, Silvana Bonilla, MD, MS3, Sarah N.. Flier, MD1, Javier A.. Villafuerte-Gálvez, MD1
1Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 2Beth Israel Deaconess Medical Center, Boston, MA; 3Boston Children's Hospital, Boston, MA
Introduction: Helicobacter pylori (HP) infection is the global leading cause of peptic ulcer disease and gastric neoplasia. In 2017, ACG guidelines changed the preferred treatment regimen from clarithromycin-based triple (CB3) to bismuth-based quadruple therapy (BB4T). There is paucity of data on predictors of eradication success (ES) in the USA, limiting potential interventions that may lead to improvement. We aimed to examine demographic and clinical factors associated with ES in the Beth Israel Deaconess Medical Center Optimization & Standardization for Treatment Outcomes in New England for HP (BOSTON-HP) cohort.
Methods: The institutional pathology database was searched for HP in gastric biopsies from 10/2016 to 07/2022. Clinical and demographic data were individually collected by two physicians from the electronic medical record with a previously validated and modified REDCap tool. Institutional Review Board approval was obtained. Fisher’s exact and χ2 tests were used as appropriate for comparison of proportions. Logistic regression was used for univariate and multivariable analysis. Post-estimation of Area Under the Curve (AUC), 95% Confidence Intervals (CI), and Standard Errors (SE) were estimated by the exact method.
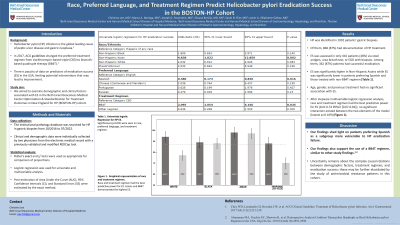
Results: HP was identified in 1002 patients’ gastric biopsies. Of them, 868 (87%) had documentation of HP treatment. Documented ES (362, 87%) or failure (54, 13%) was confirmed in 416 patients (48% of treated patients). ES was significantly higher in Non-Hispanic Asians while ES was significantly lower in patients preferring Spanish and those treated with non-BB4T regimen (Table 1). Age, gender, and previous treatment had no significant association with ES. After stepwise multivariable logistic regression analysis, race and treatment regimen had the best predictive power for ES (AUC 0.74 95%CI [0.67-0.81]); no significant interaction existed between the two elements of the model (lowest p=0.109) (Figure 1).
Discussion: Our findings shed light on patients preferring Spanish as a subgroup more vulnerable to HP eradication failure. They also support the use of a BB4T regimen. Uncertainty remains about the complex causal relations between demographic factors, treatment regimen, and eradication success; these may be further elucidated by the study of antimicrobial resistance patterns in this cohort.

Disclosures:
Christina Lee, MD1, Marco A. Noriega, MD2, Joseph D. Feuerstein, MD2, Silvana Bonilla, MD, MS3, Sarah N.. Flier, MD1, Javier A.. Villafuerte-Gálvez, MD1. P2755 - Race, Preferred Language, and Treatment Regimen Predict Helicobacter pylori Eradication Success in the BOSTON-HP Cohort, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 2Beth Israel Deaconess Medical Center, Boston, MA; 3Boston Children's Hospital, Boston, MA
Introduction: Helicobacter pylori (HP) infection is the global leading cause of peptic ulcer disease and gastric neoplasia. In 2017, ACG guidelines changed the preferred treatment regimen from clarithromycin-based triple (CB3) to bismuth-based quadruple therapy (BB4T). There is paucity of data on predictors of eradication success (ES) in the USA, limiting potential interventions that may lead to improvement. We aimed to examine demographic and clinical factors associated with ES in the Beth Israel Deaconess Medical Center Optimization & Standardization for Treatment Outcomes in New England for HP (BOSTON-HP) cohort.
Methods: The institutional pathology database was searched for HP in gastric biopsies from 10/2016 to 07/2022. Clinical and demographic data were individually collected by two physicians from the electronic medical record with a previously validated and modified REDCap tool. Institutional Review Board approval was obtained. Fisher’s exact and χ2 tests were used as appropriate for comparison of proportions. Logistic regression was used for univariate and multivariable analysis. Post-estimation of Area Under the Curve (AUC), 95% Confidence Intervals (CI), and Standard Errors (SE) were estimated by the exact method.
Results: HP was identified in 1002 patients’ gastric biopsies. Of them, 868 (87%) had documentation of HP treatment. Documented ES (362, 87%) or failure (54, 13%) was confirmed in 416 patients (48% of treated patients). ES was significantly higher in Non-Hispanic Asians while ES was significantly lower in patients preferring Spanish and those treated with non-BB4T regimen (Table 1). Age, gender, and previous treatment had no significant association with ES. After stepwise multivariable logistic regression analysis, race and treatment regimen had the best predictive power for ES (AUC 0.74 95%CI [0.67-0.81]); no significant interaction existed between the two elements of the model (lowest p=0.109) (Figure 1).
Discussion: Our findings shed light on patients preferring Spanish as a subgroup more vulnerable to HP eradication failure. They also support the use of a BB4T regimen. Uncertainty remains about the complex causal relations between demographic factors, treatment regimen, and eradication success; these may be further elucidated by the study of antimicrobial resistance patterns in this cohort.

Figure: Title: Helicobacter Pylori Eradication Success based on Both Race/Ethnicity and Treatment Regimen Simultaneously
Legend: Figure 1 is a graphical representation of eradication success (ES) based simultaneously on both race/ethnicity and treatment regimen, which consist of BB4T (bismuth quadruple therapy with tetracycline) and CB3 (Clarithromycin triple therapy). The average ES (dotted lines) for all race/ethnicity and treatment regimens was 87%. Overall, BB4T demonstrated higher ES across all race/ethnicity and treatment regimens, with Non-Hispanic Asians showing the highest ES for both treatment regimens. The error bars represent standard error.
Legend: Figure 1 is a graphical representation of eradication success (ES) based simultaneously on both race/ethnicity and treatment regimen, which consist of BB4T (bismuth quadruple therapy with tetracycline) and CB3 (Clarithromycin triple therapy). The average ES (dotted lines) for all race/ethnicity and treatment regimens was 87%. Overall, BB4T demonstrated higher ES across all race/ethnicity and treatment regimens, with Non-Hispanic Asians showing the highest ES for both treatment regimens. The error bars represent standard error.
Disclosures:
Christina Lee indicated no relevant financial relationships.
Marco Noriega indicated no relevant financial relationships.
Joseph Feuerstein indicated no relevant financial relationships.
Silvana Bonilla indicated no relevant financial relationships.
Sarah Flier indicated no relevant financial relationships.
Javier Villafuerte-Gálvez: Milky Way Biosciences – Grant/Research Support.
Christina Lee, MD1, Marco A. Noriega, MD2, Joseph D. Feuerstein, MD2, Silvana Bonilla, MD, MS3, Sarah N.. Flier, MD1, Javier A.. Villafuerte-Gálvez, MD1. P2755 - Race, Preferred Language, and Treatment Regimen Predict Helicobacter pylori Eradication Success in the BOSTON-HP Cohort, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
