Monday Poster Session
Category: Liver
P2522 - Missing the Overlap
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Rutwik Pradeep Sharma, MD
Rochester Regional Health / Unity Hospital
Rochester, NY
Presenting Author(s)
Rutwik Pradeep Sharma, MD1, Mohammed Mohammed Ahmed, MD2, Ali Jaan, MD3, Alexander Kusnik, MD4, Ahmed Shehadah, MD3, Jay Bapaye, MD3, Naga Rama Krishna Tangirala, MD2, Ari Chodos, MD5
1Rochester Regional Health / Unity Hospital, Rochester, NY; 2Rochester Regional Health, Rochester, NY; 3Rochester General Hospital, Rochester, NY; 4Rochester Regional Health, Rochester, NM; 5Unity Hospital, Rochester, NY
Introduction: Primary biliary cholangitis(PBC) is a chronic cholestatic autoimmune disease that destroys the bile ducts. Autoimmune hepatitis(AIH) is an immune-mediated inflammatory disease of the liver. PBC-AIH overlap, also known as Overlap syndrome, can be diagnosed by using the Paris criteria.
We present an atypical presentation of overlap syndrome in which the diagnosis could have been made earlier.
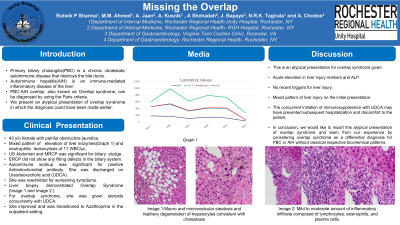
Case Description/Methods: A 43-year-old female was admitted for the evaluation of painful obstructive jaundice. Her laboratory results showed a mixed pattern of elevation of liver enzymes(AST 454U/L, ALT 665 U/L, ALP of 514U/L), elevated bilirubin(8.3mg/dl), and neutrophilic leukocytosis of 11 WBC/uL. Imaging (ultrasound and magnetic resonance pancreatography) was significant for biliary sludge and pancreatic divisum. Her ERCP did not show any filling defects in the biliary system. Given her clinical picture, she underwent a liver biopsy. Her autoimmune workup was remarkable for anti-mitochondrial antibody(AMA) positivity. She was discharged on ursodeoxycholic acid (UDCA) for PBC. She was readmitted for worsening symptoms. By that time we received her liver biopsy(Images A,B,C,D and E) results which suggested Overlap syndrome(PBC-AIH). For her overlap syndrome, she was given steroids concurrently with UDCA. She improved and was transitioned to azathioprine in the outpatient setting.
Discussion: This is an atypical presentation for overlap syndrome since our patient had an acute elevation in liver injury markers and ALP with normal levels in the recent past, no elevation of globulin, and no recent triggers for liver injury. This clinical picture did make acute pathologies such as cholangitis more likely. Given the mixed pattern of liver injury on the initial presentation of the patient we wish to suggest the consideration of overlap syndrome earlier as the pattern for PBC is cholestatic. The concurrent initiation of immunosuppression with UDCA may have prevented subsequent hospitalization and discomfort to the patient. This is a learning point from this case.
In conclusion, we would like to report this atypical presentation of overlap syndrome and learn from our experience by considering overlap syndrome as a differential diagnosis for PBC or AIH without classical respective biochemical patterns.

Disclosures:
Rutwik Pradeep Sharma, MD1, Mohammed Mohammed Ahmed, MD2, Ali Jaan, MD3, Alexander Kusnik, MD4, Ahmed Shehadah, MD3, Jay Bapaye, MD3, Naga Rama Krishna Tangirala, MD2, Ari Chodos, MD5. P2522 - Missing the Overlap, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Rochester Regional Health / Unity Hospital, Rochester, NY; 2Rochester Regional Health, Rochester, NY; 3Rochester General Hospital, Rochester, NY; 4Rochester Regional Health, Rochester, NM; 5Unity Hospital, Rochester, NY
Introduction: Primary biliary cholangitis(PBC) is a chronic cholestatic autoimmune disease that destroys the bile ducts. Autoimmune hepatitis(AIH) is an immune-mediated inflammatory disease of the liver. PBC-AIH overlap, also known as Overlap syndrome, can be diagnosed by using the Paris criteria.
We present an atypical presentation of overlap syndrome in which the diagnosis could have been made earlier.
Case Description/Methods: A 43-year-old female was admitted for the evaluation of painful obstructive jaundice. Her laboratory results showed a mixed pattern of elevation of liver enzymes(AST 454U/L, ALT 665 U/L, ALP of 514U/L), elevated bilirubin(8.3mg/dl), and neutrophilic leukocytosis of 11 WBC/uL. Imaging (ultrasound and magnetic resonance pancreatography) was significant for biliary sludge and pancreatic divisum. Her ERCP did not show any filling defects in the biliary system. Given her clinical picture, she underwent a liver biopsy. Her autoimmune workup was remarkable for anti-mitochondrial antibody(AMA) positivity. She was discharged on ursodeoxycholic acid (UDCA) for PBC. She was readmitted for worsening symptoms. By that time we received her liver biopsy(Images A,B,C,D and E) results which suggested Overlap syndrome(PBC-AIH). For her overlap syndrome, she was given steroids concurrently with UDCA. She improved and was transitioned to azathioprine in the outpatient setting.
Discussion: This is an atypical presentation for overlap syndrome since our patient had an acute elevation in liver injury markers and ALP with normal levels in the recent past, no elevation of globulin, and no recent triggers for liver injury. This clinical picture did make acute pathologies such as cholangitis more likely. Given the mixed pattern of liver injury on the initial presentation of the patient we wish to suggest the consideration of overlap syndrome earlier as the pattern for PBC is cholestatic. The concurrent initiation of immunosuppression with UDCA may have prevented subsequent hospitalization and discomfort to the patient. This is a learning point from this case.
In conclusion, we would like to report this atypical presentation of overlap syndrome and learn from our experience by considering overlap syndrome as a differential diagnosis for PBC or AIH without classical respective biochemical patterns.

Figure: Image A and B: Macro vesicular and micro vesicular steatosis and feathery degeneration of hepatocytes consistent with cholestasis
Image C,D and E: Mild to moderate amount of inflammatory infiltrate composed of lymphocytes, eosinophils, and plasma cells
Image C,D and E: Mild to moderate amount of inflammatory infiltrate composed of lymphocytes, eosinophils, and plasma cells
Disclosures:
Rutwik Pradeep Sharma indicated no relevant financial relationships.
Mohammed Mohammed Ahmed indicated no relevant financial relationships.
Ali Jaan indicated no relevant financial relationships.
Alexander Kusnik indicated no relevant financial relationships.
Ahmed Shehadah indicated no relevant financial relationships.
Jay Bapaye indicated no relevant financial relationships.
Naga Rama Krishna Tangirala indicated no relevant financial relationships.
Ari Chodos indicated no relevant financial relationships.
Rutwik Pradeep Sharma, MD1, Mohammed Mohammed Ahmed, MD2, Ali Jaan, MD3, Alexander Kusnik, MD4, Ahmed Shehadah, MD3, Jay Bapaye, MD3, Naga Rama Krishna Tangirala, MD2, Ari Chodos, MD5. P2522 - Missing the Overlap, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
