Monday Poster Session
Category: Liver
P2533 - Small for Size Syndrome Following Living Donor Liver Transplantation
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Tabassum F. Chowdhury, BS
Wayne State University
Troy, MI
Presenting Author(s)
Tabassum F.. Chowdhury, BS1, Syed-Mohammed Jafri, MD2
1Wayne State University, Troy, MI; 2Henry Ford Health System, Detroit, MI
Introduction: We present a unique case of a patient with small-for-size syndrome (SFSS) following a living donor liver transplant (LDLT) for nonalcoholic steatohepatitis (NASH) cirrhosis.
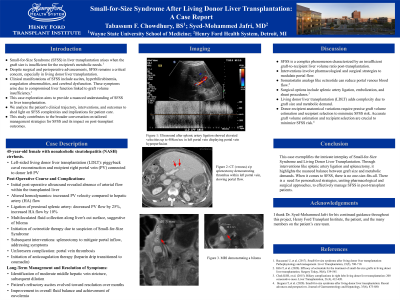
Case Description/Methods: A 45 year old female with NASH cirrhosis with hepatic encephalopathy, ascites, esophageal varices, jaundice, and anemia presents for a liver transplant. Past abdominal surgical history is significant for c-section, an open colectomy for diverticulitis, and an incisional hernia with mesh after the colon surgery. Since her liver disease diagnosis, the patient has not consumed any alcohol. The patient then undergoes a left-sided LDLT, with a piggyback caval reconstruction and recipient right portal vein (PV) connected to donor left PV. On post-op day 1, ultrasound shows no flow within the liver from the artery, so an exploration is performed. PV velocity was increased in relation to hepatic artery (HA) flow. After the proximal splenic artery was doubly ligated, PV flow decreased by 25% and HA flow increased by 10%. No outflow obstruction is observed. A month later, there is multiloculated fluid collection along the cut surface of the liver consistent with biloma. With the concern of SFSS, the patient is started on octreotide. Two months post-op, the patient continues to have lower extremity edema and pleural effusion, not responding to diuretics. While evaluating for the cause of the ascites and pleural effusion, there is a small hepatic outflow stenosis which is dilated. A splenectomy is then performed to decrease inflow into the portal system. Two days post-splenectomy, she develops PV thrombosis and is started on heparin drip transitioned to coumadin. Repeat hepatic venogram two months later shows moderate middle hepatic vein stricture, which was dilated. Patient had a prolonged period of refractory ascites over the next year, but eventually improved with current euvolemia.
Discussion: SFSS is a clinical syndrome following liver transplant where the liver fails to function at a level to meet the body’s metabolic demands. In the absence of ischemia, SFSS presents as ascites, hyperbilirubinemia, prolonged prothrombin time, or alterations in cerebral function. SFSS can be managed medically or surgically. For surgical reduction of portal inflow, shunts, splenic artery ligation, or a splenectomy may be performed. For medical management, somatostatin is helpful in reducing the portal venous blood flow.
Disclosures:
Tabassum F.. Chowdhury, BS1, Syed-Mohammed Jafri, MD2. P2533 - Small for Size Syndrome Following Living Donor Liver Transplantation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wayne State University, Troy, MI; 2Henry Ford Health System, Detroit, MI
Introduction: We present a unique case of a patient with small-for-size syndrome (SFSS) following a living donor liver transplant (LDLT) for nonalcoholic steatohepatitis (NASH) cirrhosis.
Case Description/Methods: A 45 year old female with NASH cirrhosis with hepatic encephalopathy, ascites, esophageal varices, jaundice, and anemia presents for a liver transplant. Past abdominal surgical history is significant for c-section, an open colectomy for diverticulitis, and an incisional hernia with mesh after the colon surgery. Since her liver disease diagnosis, the patient has not consumed any alcohol. The patient then undergoes a left-sided LDLT, with a piggyback caval reconstruction and recipient right portal vein (PV) connected to donor left PV. On post-op day 1, ultrasound shows no flow within the liver from the artery, so an exploration is performed. PV velocity was increased in relation to hepatic artery (HA) flow. After the proximal splenic artery was doubly ligated, PV flow decreased by 25% and HA flow increased by 10%. No outflow obstruction is observed. A month later, there is multiloculated fluid collection along the cut surface of the liver consistent with biloma. With the concern of SFSS, the patient is started on octreotide. Two months post-op, the patient continues to have lower extremity edema and pleural effusion, not responding to diuretics. While evaluating for the cause of the ascites and pleural effusion, there is a small hepatic outflow stenosis which is dilated. A splenectomy is then performed to decrease inflow into the portal system. Two days post-splenectomy, she develops PV thrombosis and is started on heparin drip transitioned to coumadin. Repeat hepatic venogram two months later shows moderate middle hepatic vein stricture, which was dilated. Patient had a prolonged period of refractory ascites over the next year, but eventually improved with current euvolemia.
Discussion: SFSS is a clinical syndrome following liver transplant where the liver fails to function at a level to meet the body’s metabolic demands. In the absence of ischemia, SFSS presents as ascites, hyperbilirubinemia, prolonged prothrombin time, or alterations in cerebral function. SFSS can be managed medically or surgically. For surgical reduction of portal inflow, shunts, splenic artery ligation, or a splenectomy may be performed. For medical management, somatostatin is helpful in reducing the portal venous blood flow.
Disclosures:
Tabassum Chowdhury indicated no relevant financial relationships.
Syed-Mohammed Jafri: Gilead, Takeda, Abbvie – Advisor or Review Panel Member, Speakers Bureau.
Tabassum F.. Chowdhury, BS1, Syed-Mohammed Jafri, MD2. P2533 - Small for Size Syndrome Following Living Donor Liver Transplantation, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
