Monday Poster Session
Category: Interventional Endoscopy
P2301 - Depth of Resection With Different EMR Techniques for Large Colorectal Polyps
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
- AS
Andy Silva-Santisteban, MD
Beth Israel Deaconess Medical Center
Brighton, Massachusetts
Presenting Author(s)
Sultan Mahmood, MD1, Andy Silva-Santisteban, MD2, Monika Vyas, MD1, Samuel Igbinedion, MD3, Erik Holzwanger, MD1, Mandeep Sawhney, MD, MS1, Douglas Pleskow, MD, FACG4, Tyler Berzin, MD, FACG1, Moamen Gabr, MD, MSc,1
1Beth Israel Deaconess Medical Center, Boston, MA; 2Beth Israel Deaconess Medical Center, Brighton, MA; 3Center for Advanced Endoscopy, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 4BIDMC, Boston, MA
Introduction: Endoscopic mucosal resection (EMR) is the preferred method for removal of large colon polyps ( >15mm). Traditional EMR (t-EMR) is the most common method and usually involves submucosal injection of a lifting agent. Recently newer techniques like Underwater EMR (u-EMR) and piecemeal cold snare EMR (c-EMR) are gaining popularity. There are limited studies looking at the depth of resection between different EMR techniques.
Methods: Consecutive patients who underwent t-EMR, u-EMR and c-EMR at the Center for advanced endoscopy at our institution during the year 2022 were included in study. We estimated that approximately 20 patients for each arm will be needed for the study with an effect size of 40% with minimum confidence interval of 95%, alpha of 0.05 and power of 80%. Pathology slides of the polyp were reviewed to determine the depth of resection and the presence of submucosa and muscularis mucosae in the samples. The measurements were made on an Olympus BX43 microscope using a micrometer scale. Depth of submucosa is measured from the base of muscularis mucosae to the cauterized edge of submucosa.
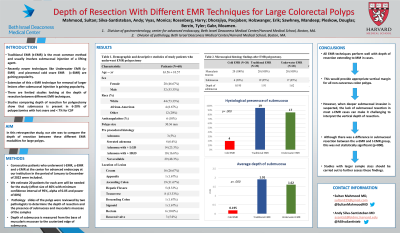
Results: During the study period, 60 patients underwent EMR. The average age of study patients was 63.5 years, 46.6% were women, and 73.3% were of white descent. The average polyp size was 30.3 mm. The majority of polyps with known pre-procedural histology were adenomas with low-grade dysplasia (23.3%) and the most common location of lesions was in ascending colon (31.6%) (fig.1, Table 1). The depth of resection extended to the muscularis mucosa in all of the EMR specimens. Submucosa was present in 20% of c-EMR cases, 95% of t-EMR cases and 85% of u-EMR cases. c-EMR, t-EMR and u-EMR average depth of resection was 0.195, 1.91 and 1.62 mm, respectively (fig.1, Table 2). Difference between T-EMR and u-EMR for submucosal resection of large polyp removal was not significant (p=0.156).
Discussion: All EMR techniques perform well with depth of resection extending to muscularis mucosae in all cases. This would provide appropriate vertical margin for all non-cancerous colon polyps. However, when deeper submucosal invasion is suspected, c-EMR shouldn’t be used as it lacks appropriate vertical resection margins. Although there was a difference in submucosal resection between the u-EMR and t-EMR group, this was not statistically significant. Studies with larger sample sizes should be carried out to further assess these findings.

Disclosures:
Sultan Mahmood, MD1, Andy Silva-Santisteban, MD2, Monika Vyas, MD1, Samuel Igbinedion, MD3, Erik Holzwanger, MD1, Mandeep Sawhney, MD, MS1, Douglas Pleskow, MD, FACG4, Tyler Berzin, MD, FACG1, Moamen Gabr, MD, MSc,1. P2301 - Depth of Resection With Different EMR Techniques for Large Colorectal Polyps, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Boston, MA; 2Beth Israel Deaconess Medical Center, Brighton, MA; 3Center for Advanced Endoscopy, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA; 4BIDMC, Boston, MA
Introduction: Endoscopic mucosal resection (EMR) is the preferred method for removal of large colon polyps ( >15mm). Traditional EMR (t-EMR) is the most common method and usually involves submucosal injection of a lifting agent. Recently newer techniques like Underwater EMR (u-EMR) and piecemeal cold snare EMR (c-EMR) are gaining popularity. There are limited studies looking at the depth of resection between different EMR techniques.
Methods: Consecutive patients who underwent t-EMR, u-EMR and c-EMR at the Center for advanced endoscopy at our institution during the year 2022 were included in study. We estimated that approximately 20 patients for each arm will be needed for the study with an effect size of 40% with minimum confidence interval of 95%, alpha of 0.05 and power of 80%. Pathology slides of the polyp were reviewed to determine the depth of resection and the presence of submucosa and muscularis mucosae in the samples. The measurements were made on an Olympus BX43 microscope using a micrometer scale. Depth of submucosa is measured from the base of muscularis mucosae to the cauterized edge of submucosa.
Results: During the study period, 60 patients underwent EMR. The average age of study patients was 63.5 years, 46.6% were women, and 73.3% were of white descent. The average polyp size was 30.3 mm. The majority of polyps with known pre-procedural histology were adenomas with low-grade dysplasia (23.3%) and the most common location of lesions was in ascending colon (31.6%) (fig.1, Table 1). The depth of resection extended to the muscularis mucosa in all of the EMR specimens. Submucosa was present in 20% of c-EMR cases, 95% of t-EMR cases and 85% of u-EMR cases. c-EMR, t-EMR and u-EMR average depth of resection was 0.195, 1.91 and 1.62 mm, respectively (fig.1, Table 2). Difference between T-EMR and u-EMR for submucosal resection of large polyp removal was not significant (p=0.156).
Discussion: All EMR techniques perform well with depth of resection extending to muscularis mucosae in all cases. This would provide appropriate vertical margin for all non-cancerous colon polyps. However, when deeper submucosal invasion is suspected, c-EMR shouldn’t be used as it lacks appropriate vertical resection margins. Although there was a difference in submucosal resection between the u-EMR and t-EMR group, this was not statistically significant. Studies with larger sample sizes should be carried out to further assess these findings.

Figure: Figure 1: Table 1) Demographic and descriptive statistics of study patients who underwent EMR polypectomy. Table 2) Microscopical histology findings after EMR polypectomy.
Disclosures:
Sultan Mahmood indicated no relevant financial relationships.
Andy Silva-Santisteban indicated no relevant financial relationships.
Monika Vyas indicated no relevant financial relationships.
Samuel Igbinedion indicated no relevant financial relationships.
Erik Holzwanger indicated no relevant financial relationships.
Mandeep Sawhney: Allurion – Stock Options. Immunovia Inc. – Consultant. Marlborough, MA – Consultant.
Douglas Pleskow: Boston Scientific – Consultant. Fuji – Consultant. Olympus – Consultant.
Tyler Berzin: Boston Scientific – Consultant. Fuji – Consultant. Medtronic – Consultant.
Moamen Gabr: Adaptive Endo – Consultant. Boston Scientific – Consultant. ConMed – Consultant. Fuji – Consultant. Medtronic – Consultant. Olympus – Consultant.
Sultan Mahmood, MD1, Andy Silva-Santisteban, MD2, Monika Vyas, MD1, Samuel Igbinedion, MD3, Erik Holzwanger, MD1, Mandeep Sawhney, MD, MS1, Douglas Pleskow, MD, FACG4, Tyler Berzin, MD, FACG1, Moamen Gabr, MD, MSc,1. P2301 - Depth of Resection With Different EMR Techniques for Large Colorectal Polyps, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
