Monday Poster Session
Category: Interventional Endoscopy
P2302 - Outcomes and Long-Term Follow-Up for Endoscopic Repair of Sleeve Gastrectomy Anastomotic Leaks
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Khalid Fahoum, MD, MSc
NYU Grossman School of Medicine
New York, NY
Presenting Author(s)
Khalid Fahoum, MD, MSc1, Tamara Kahan, MD, MPA1, Matthew Fasullo, DO2, Ki-Yoon Kim, MD3, Lauren Khanna, MD3, Gregory Haber, MD4, Paresh C. Shah, MD5, Tamas Gonda, MD1
1NYU Grossman School of Medicine, New York, NY; 2NYU Langone Medical Center, New York, NY; 3NYU Langone, New York, NY; 4NYU, New York, NY; 5New York-Presbyterian/Weill Cornell, New York, NY
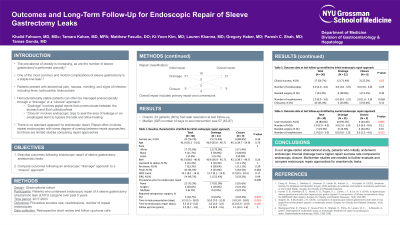
Introduction: Anastomotic leaks following sleeve gastrectomy have significant morbidity and mortality. Few studies compare endoscopic approaches to repairing sleeve leaks. Our goal was to characterize these approaches and describe outcomes following repair.
Methods: All patients who underwent endoscopic repair of a sleeve gastrectomy anastomotic leak from 2017-2023 at our center were identified. Procedure reports were reviewed to characterize endoscopic repairs and long-term outcome data was obtained from the electronic medical record and patient phone calls. Repair approach was classified as drainage when transmural stents were placed and as closure when clips, sutures, or an intraluminal stent was placed.
Results: A total of 30 patients were included. The majority were female (74%) and White (75%), with a median (interquartile range - IQR) age of 41.0 (35.2-51.0) and median (IQR) pre-sleeve BMI of 41.0 (38.0-46.4). The median (IQR) length of time between sleeve gastrectomy and leak presentation was 9.5 (5.5 - 28.0) days. The majority of patients (70%) initially underwent drainage while the rest underwent closure. The median (IQR) follow-up time was 1.2 (0.65 -1.64) years. Success rates for the initial repair approach without crossover or requiring surgery were 71.4% for drainage and 22.2% for closure (p = 0.02). Of note, 3/6 patients who failed an initial drainage approach had a gastropulmonary fistula. There were 5 conversions to closure in the drainage group (23.8%) and 5 conversions to drainage in the closure group (55.6%) (p = 0.12). The overall success rate of a drainage approach (including primary drainage and conversion to drainage) was 95.2% whereas the overall success rate of a closure approach was 44.4% (p=0.005). An overall drainage approach was associated with fewer readmissions (median [IQR] of 0.0 [0.0-1.0]) compared to an overall closure approach (3.0 [1.0-4.0]) (p = 0.013). Overall, 24 patients (80%) had leak resolution at last follow-up and median (IQR) number of days to last intervention was 57 (45-87). Median (IQR) number of repeat endoscopies was 2 (1-3).
Discussion: Our study highlights outcomes for endoscopic repair of anastomotic leaks following sleeve gastrectomy. Drainage was associated with a higher overall success rate and fewer readmissions when conversions to drainage were included. Half of patients who failed drainage had a gastropulmonary fistula. Multicenter studies are needed to further evaluate and compare endoscopic repair approaches for anastomotic leaks.
Disclosures:
Khalid Fahoum, MD, MSc1, Tamara Kahan, MD, MPA1, Matthew Fasullo, DO2, Ki-Yoon Kim, MD3, Lauren Khanna, MD3, Gregory Haber, MD4, Paresh C. Shah, MD5, Tamas Gonda, MD1. P2302 - Outcomes and Long-Term Follow-Up for Endoscopic Repair of Sleeve Gastrectomy Anastomotic Leaks, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1NYU Grossman School of Medicine, New York, NY; 2NYU Langone Medical Center, New York, NY; 3NYU Langone, New York, NY; 4NYU, New York, NY; 5New York-Presbyterian/Weill Cornell, New York, NY
Introduction: Anastomotic leaks following sleeve gastrectomy have significant morbidity and mortality. Few studies compare endoscopic approaches to repairing sleeve leaks. Our goal was to characterize these approaches and describe outcomes following repair.
Methods: All patients who underwent endoscopic repair of a sleeve gastrectomy anastomotic leak from 2017-2023 at our center were identified. Procedure reports were reviewed to characterize endoscopic repairs and long-term outcome data was obtained from the electronic medical record and patient phone calls. Repair approach was classified as drainage when transmural stents were placed and as closure when clips, sutures, or an intraluminal stent was placed.
Results: A total of 30 patients were included. The majority were female (74%) and White (75%), with a median (interquartile range - IQR) age of 41.0 (35.2-51.0) and median (IQR) pre-sleeve BMI of 41.0 (38.0-46.4). The median (IQR) length of time between sleeve gastrectomy and leak presentation was 9.5 (5.5 - 28.0) days. The majority of patients (70%) initially underwent drainage while the rest underwent closure. The median (IQR) follow-up time was 1.2 (0.65 -1.64) years. Success rates for the initial repair approach without crossover or requiring surgery were 71.4% for drainage and 22.2% for closure (p = 0.02). Of note, 3/6 patients who failed an initial drainage approach had a gastropulmonary fistula. There were 5 conversions to closure in the drainage group (23.8%) and 5 conversions to drainage in the closure group (55.6%) (p = 0.12). The overall success rate of a drainage approach (including primary drainage and conversion to drainage) was 95.2% whereas the overall success rate of a closure approach was 44.4% (p=0.005). An overall drainage approach was associated with fewer readmissions (median [IQR] of 0.0 [0.0-1.0]) compared to an overall closure approach (3.0 [1.0-4.0]) (p = 0.013). Overall, 24 patients (80%) had leak resolution at last follow-up and median (IQR) number of days to last intervention was 57 (45-87). Median (IQR) number of repeat endoscopies was 2 (1-3).
Discussion: Our study highlights outcomes for endoscopic repair of anastomotic leaks following sleeve gastrectomy. Drainage was associated with a higher overall success rate and fewer readmissions when conversions to drainage were included. Half of patients who failed drainage had a gastropulmonary fistula. Multicenter studies are needed to further evaluate and compare endoscopic repair approaches for anastomotic leaks.
Disclosures:
Khalid Fahoum indicated no relevant financial relationships.
Tamara Kahan indicated no relevant financial relationships.
Matthew Fasullo indicated no relevant financial relationships.
Ki-Yoon Kim indicated no relevant financial relationships.
Lauren Khanna indicated no relevant financial relationships.
Gregory Haber: BSC – Consultant. Digma – Consultant. Erbe – Consultant. Medtronic – Consultant. Microtech – Consultant. Olympus – Consultant. Ovesco – Consultant.
Paresh Shah: CareCentra – Owner/Ownership Interest. Intuitive Surgical – Advisory Committee/Board Member.
Tamas Gonda indicated no relevant financial relationships.
Khalid Fahoum, MD, MSc1, Tamara Kahan, MD, MPA1, Matthew Fasullo, DO2, Ki-Yoon Kim, MD3, Lauren Khanna, MD3, Gregory Haber, MD4, Paresh C. Shah, MD5, Tamas Gonda, MD1. P2302 - Outcomes and Long-Term Follow-Up for Endoscopic Repair of Sleeve Gastrectomy Anastomotic Leaks, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
