Monday Poster Session
Category: Interventional Endoscopy
P2306 - Curative Resection of T1a Esophageal Inlet Patch Adenocarcinoma With Traction-Assisted Endoscopic Submucosal Dissection
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio
Firas Bahdi, MD
David Geffen School of Medicine at University of California Los Angeles
Los Angeles, CA
Presenting Author(s)
Firas Bahdi, MD1, Robert Tamai, MD1, David Y.. Lu, MD1, Daniel D.. Eshtiaghpour, MD1, Adarsh Thaker, MD2, Alireza Sedarat, MD2
1David Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA; 2UCLA, Los Angeles, CA
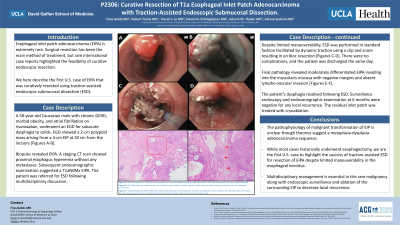
Introduction: Esophageal inlet patch adenocarcinoma (EIPA) is extremely rare. Surgical resection has been the main method of treatment, but rare international case reports highlighted the feasibility of curative endoscopic resection. We here describe the first U.S. case of EIPA that was curatively resected using traction-assisted endoscopic submucosal dissection (ESD).
Case Description/Methods: A 58-year-old Caucasian male with chronic GERD, morbid obesity, and atrial fibrillation on rivaroxaban, underwent an EGD for subacute dysphagia to solids. EGD showed a 2-cm polypoid mass arising from a 4-cm EIP at 20 cm from the incisors [Figures A-B]. Biopsies revealed EIPA. A staging CT scan showed proximal esophagus hyperemia without any metastases. Subsequent endosonographic examination suggested a T1aN0Mx EIPA. Following multidisciplinary discussion, the patient was referred for ESD. Despite limited maneuverability in the esophageal introitus, ESD was performed in standard fashion (marking with coagulation dots, submucosal lifting using methylene-blue-tinted hetastarch, mucosal incision, and submucosal dissection) facilitated by dynamic traction using a clip and snare resulting in en bloc resection [Figures C-D]. There were no complications, and the patient was discharged the same day. Final pathological examination revealed moderately differentiated EIPA invading into the muscularis mucosa with negative margins and absent lymphovascular invasion suggestive of curative resection [Figures E-F]. At follow up, the patient’s dysphagia resolved, and surveillance endoscopy is pending with radiofrequency ablation (RFA) of any residual EIP.
Discussion: The pathophysiology of malignant transformation of EIP is unclear though theories suggest a metaplasia-dysplasia-adenocarcinoma sequence. While most cases historically underwent esophagectomy, we are the first U.S. case to highlight the success of traction-assisted ESD for resection of EIPA. Traction-assistance was crucial for visualization of dissection plan given limited maneuverability in the esophageal introitus. Multidisciplinary management is essential in this rare malignancy along with endoscopic surveillance and consideration of RFA of the surrounding EIP to decrease local recurrence.

Disclosures:
Firas Bahdi, MD1, Robert Tamai, MD1, David Y.. Lu, MD1, Daniel D.. Eshtiaghpour, MD1, Adarsh Thaker, MD2, Alireza Sedarat, MD2. P2306 - Curative Resection of T1a Esophageal Inlet Patch Adenocarcinoma With Traction-Assisted Endoscopic Submucosal Dissection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1David Geffen School of Medicine at University of California Los Angeles, Los Angeles, CA; 2UCLA, Los Angeles, CA
Introduction: Esophageal inlet patch adenocarcinoma (EIPA) is extremely rare. Surgical resection has been the main method of treatment, but rare international case reports highlighted the feasibility of curative endoscopic resection. We here describe the first U.S. case of EIPA that was curatively resected using traction-assisted endoscopic submucosal dissection (ESD).
Case Description/Methods: A 58-year-old Caucasian male with chronic GERD, morbid obesity, and atrial fibrillation on rivaroxaban, underwent an EGD for subacute dysphagia to solids. EGD showed a 2-cm polypoid mass arising from a 4-cm EIP at 20 cm from the incisors [Figures A-B]. Biopsies revealed EIPA. A staging CT scan showed proximal esophagus hyperemia without any metastases. Subsequent endosonographic examination suggested a T1aN0Mx EIPA. Following multidisciplinary discussion, the patient was referred for ESD. Despite limited maneuverability in the esophageal introitus, ESD was performed in standard fashion (marking with coagulation dots, submucosal lifting using methylene-blue-tinted hetastarch, mucosal incision, and submucosal dissection) facilitated by dynamic traction using a clip and snare resulting in en bloc resection [Figures C-D]. There were no complications, and the patient was discharged the same day. Final pathological examination revealed moderately differentiated EIPA invading into the muscularis mucosa with negative margins and absent lymphovascular invasion suggestive of curative resection [Figures E-F]. At follow up, the patient’s dysphagia resolved, and surveillance endoscopy is pending with radiofrequency ablation (RFA) of any residual EIP.
Discussion: The pathophysiology of malignant transformation of EIP is unclear though theories suggest a metaplasia-dysplasia-adenocarcinoma sequence. While most cases historically underwent esophagectomy, we are the first U.S. case to highlight the success of traction-assisted ESD for resection of EIPA. Traction-assistance was crucial for visualization of dissection plan given limited maneuverability in the esophageal introitus. Multidisciplinary management is essential in this rare malignancy along with endoscopic surveillance and consideration of RFA of the surrounding EIP to decrease local recurrence.

Figure: Figures A-B: EGD demonstrated a 2-cm polypoid mass arising from a proximal esophageal inlet patch under high-definition white light endoscopy (A), and narrow band imaging (B).
Figures C-D: ESD of the lesion with traction assistance by a clip and snare resulting in complete resection with post-resection defect involving around the third of the esophageal circumference.
Figures E-F: Histopathological examination (H&E, 40x) revealing heterotopic gastric oxyntic glands (E, red box) at one edge of the mass, consistent with inlet patch origin. At the base of the mass, invasive adenocarcinoma (F, at right) encroaching on the thin pink bands of the muscularis mucosa (F, red arrows).
Figures C-D: ESD of the lesion with traction assistance by a clip and snare resulting in complete resection with post-resection defect involving around the third of the esophageal circumference.
Figures E-F: Histopathological examination (H&E, 40x) revealing heterotopic gastric oxyntic glands (E, red box) at one edge of the mass, consistent with inlet patch origin. At the base of the mass, invasive adenocarcinoma (F, at right) encroaching on the thin pink bands of the muscularis mucosa (F, red arrows).
Disclosures:
Firas Bahdi indicated no relevant financial relationships.
Robert Tamai indicated no relevant financial relationships.
David Lu indicated no relevant financial relationships.
Daniel Eshtiaghpour indicated no relevant financial relationships.
Adarsh Thaker: Apollo Endosurgery – Advisory Committee/Board Member, Consultant. Boston Scientific Corporation – Consultant, Speakers Bureau. Neptune Medical – Consultant. Steris – Consultant.
Alireza Sedarat: Boston Scientific – Consultant.
Firas Bahdi, MD1, Robert Tamai, MD1, David Y.. Lu, MD1, Daniel D.. Eshtiaghpour, MD1, Adarsh Thaker, MD2, Alireza Sedarat, MD2. P2306 - Curative Resection of T1a Esophageal Inlet Patch Adenocarcinoma With Traction-Assisted Endoscopic Submucosal Dissection, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
