Monday Poster Session
Category: Interventional Endoscopy
P2313 - Advanced Endoscopic Management of Complex Post-Esophagectomy Leaks: A Case Series
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Munraj Singh, MD
LSU Health Sciences Center
New Orleans, LA
Presenting Author(s)
Munraj Singh, MD, Catherine Hudson, MD, MPH
LSU Health Sciences Center, New Orleans, LA
Introduction: Esophagectomy is the mainstay of management in patients with advanced esophageal cancer but carries significant risk of morbidity and mortality. The incidence of anastomotic leak complications has been reported to occur in up to 25% of cases depending on the site of anastomosis. While conventional treatment for anastomotic leak includes conservative therapy and surgical intervention; non-invasive endoscopic techniques such as stenting and endoscopic vacuum therapy (EVT) have become more widely used. Herein we present 3 cases of complex post-esophagectomy anastomotic leaks managed with a combination of endoscopic stents and EVT.
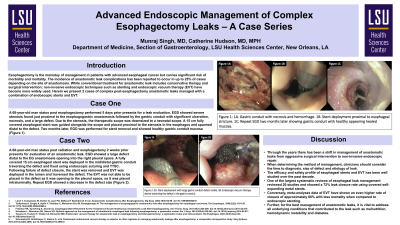
Case Description/Methods: A 68 yo man status post radiation and esophagectomy 2 weeks prior presents for evaluation of an anastomotic leak. EGD showed a large defect distal to the EG anastomosis opening into the right pleural space. This space had copious amount of fluid and sutures that had become unraveled at the anastomosis site. The pleural space was irrigated and suctioned to reveal the chest tube entering through the chest wall. Following the washout, the unraveled suture that had been used to approximate the anastomosis was found and removed endoscopically. Then a fully covered 15 cm esophageal stent was deployed in the mid/distal gastric conduit traversing the defect and fixed using endoscopic suturing and TTSC. Following failure of defect closure, the stent was removed and EVT was deployed in the lumen and traversed the defect. Follow subsequent EVT exchanges, repeat EGD showed a decrease in the defect size. Two further cases highlight endoscopic stent placement complicated by esophageal strictures.
Discussion: Through the years there has been a shift in management of anastomotic leaks from aggressive surgical intervention to non-invasive endoscopic repair. The efficacy and safety profile of esophageal stents and EVT has been well studied over the past decade. Meta-analyses of esophageal leak management show a 70-80% closure rate for both covered self-expanding stents and EVT, with the later shown have lower rates of mortality when compared to endoscopic stenting. Further, for the best management of anastomotic leaks, it is vital to address all underlying conditions that contributed to the leak such as malnutrition, hemodynamic instability and diabetes.

Disclosures:
Munraj Singh, MD, Catherine Hudson, MD, MPH. P2313 - Advanced Endoscopic Management of Complex Post-Esophagectomy Leaks: A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
LSU Health Sciences Center, New Orleans, LA
Introduction: Esophagectomy is the mainstay of management in patients with advanced esophageal cancer but carries significant risk of morbidity and mortality. The incidence of anastomotic leak complications has been reported to occur in up to 25% of cases depending on the site of anastomosis. While conventional treatment for anastomotic leak includes conservative therapy and surgical intervention; non-invasive endoscopic techniques such as stenting and endoscopic vacuum therapy (EVT) have become more widely used. Herein we present 3 cases of complex post-esophagectomy anastomotic leaks managed with a combination of endoscopic stents and EVT.
Case Description/Methods: A 68 yo man status post radiation and esophagectomy 2 weeks prior presents for evaluation of an anastomotic leak. EGD showed a large defect distal to the EG anastomosis opening into the right pleural space. This space had copious amount of fluid and sutures that had become unraveled at the anastomosis site. The pleural space was irrigated and suctioned to reveal the chest tube entering through the chest wall. Following the washout, the unraveled suture that had been used to approximate the anastomosis was found and removed endoscopically. Then a fully covered 15 cm esophageal stent was deployed in the mid/distal gastric conduit traversing the defect and fixed using endoscopic suturing and TTSC. Following failure of defect closure, the stent was removed and EVT was deployed in the lumen and traversed the defect. Follow subsequent EVT exchanges, repeat EGD showed a decrease in the defect size. Two further cases highlight endoscopic stent placement complicated by esophageal strictures.
Discussion: Through the years there has been a shift in management of anastomotic leaks from aggressive surgical intervention to non-invasive endoscopic repair. The efficacy and safety profile of esophageal stents and EVT has been well studied over the past decade. Meta-analyses of esophageal leak management show a 70-80% closure rate for both covered self-expanding stents and EVT, with the later shown have lower rates of mortality when compared to endoscopic stenting. Further, for the best management of anastomotic leaks, it is vital to address all underlying conditions that contributed to the leak such as malnutrition, hemodynamic instability and diabetes.

Figure: Figure 1: 1A shows stent deployment with large gastric conduit defect visible. 1B shows endoscopic vacuum therapy device deployed intra-luminally.
Disclosures:
Munraj Singh indicated no relevant financial relationships.
Catherine Hudson indicated no relevant financial relationships.
Munraj Singh, MD, Catherine Hudson, MD, MPH. P2313 - Advanced Endoscopic Management of Complex Post-Esophagectomy Leaks: A Case Series, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
