Monday Poster Session
Category: GI Bleeding
P2099 - Seeing the Unseen: Management of a Jejunal Variceal Bleed with Endoscopic Sclerosing Therapy Followed by Coil Embolization
Monday, October 23, 2023
10:30 AM - 4:15 PM PT
Location: Exhibit Hall
Has Audio

Ibrahim Yaghnam, MD
Penn State University Milton S. Hershey Medical Center
Hummelstown, PA
Presenting Author(s)
Scott Weismiller, MD1, Ibrahim Yaghnam, MD2, Ian Schreibman, MD1
1Hershey Medical Center, Hershey, PA; 2Penn State University Milton S. Hershey Medical Center, Hummelstown, PA
Introduction: Isolated jejunal varices are an uncommon manifestation of portal hypertension and a rare cause of hemodynamically significant gastrointestinal bleeding. Cases in cirrhotic patients with portal hypertension and a history of abdominal surgery have been reported. Identifying and managing these bleeding varices are complicated and may require advanced techniques, such as double balloon enteroscopy (DBE), where banding is not compatible with the endoscopes. Often co-management with radiology for coil embolization or surgical resection may be required.
We report a case of successful control of a jejunal variceal bleed by identifying the varix on CT angiography (CTA), treating it endoscopically with sclerosing agent with subsequent placement of a fiducial clip, followed by definitive treatment with coil embolization.
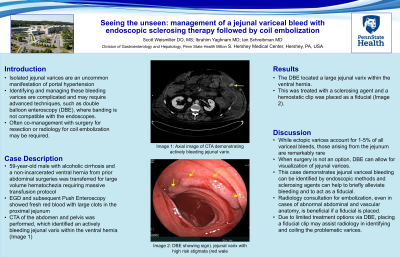
Case Description/Methods: A 59-year-old male with alcoholic cirrhosis and a non-incarcerated ventral hernia from prior abdominal surgeries was transferred for large volume hematochezia requiring massive transfusion protocol and pressor support in the medical intensive care unit. Esophagogastroduodenoscopy (EGD) showed fresh red blood with large clots in the proximal jejunum with no active bleed. A CTA of the abdomen and pelvis was performed, which identified an actively bleeding jejunal varix within the ventral hernia (Image 1).
A DBE located a large jejunal varix within the ventral hernia. This was treated with a sclerosing agent and placing a hemostatic clip as a fiducial. Although successful, we consulted radiology for embolization due to the high-risk features of the varix (Image 2). Ten coils were deployed within the distal branches of the superior mesenteric vein (SMV). Initial access to the inferior mesenteric vein created iatrogenic venous injury leading to bleeding in the small bowel, requiring the left inferior epigastric vein to access to the peripherals of the superior mesenteric vein. Surgery was consulted, but determined the patient was not a surgical candidate.
Discussion: While ectopic varices account for 1-5% of all variceal bleeds, those arising from the jejunum are remarkably rare. This case demonstrates jejunal variceal bleeding can be treated by endoscopic evaluation and embolization, even in cases of abnormal abdominal and vascular anatomy.
When surgery is not an option, DBE can allow for visualization of jejunal varices. Due to lack of treatment options via DBE, placing a fiducial clip may assist radiology in identifying and coiling the problematic varices.

Disclosures:
Scott Weismiller, MD1, Ibrahim Yaghnam, MD2, Ian Schreibman, MD1. P2099 - Seeing the Unseen: Management of a Jejunal Variceal Bleed with Endoscopic Sclerosing Therapy Followed by Coil Embolization, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Hershey Medical Center, Hershey, PA; 2Penn State University Milton S. Hershey Medical Center, Hummelstown, PA
Introduction: Isolated jejunal varices are an uncommon manifestation of portal hypertension and a rare cause of hemodynamically significant gastrointestinal bleeding. Cases in cirrhotic patients with portal hypertension and a history of abdominal surgery have been reported. Identifying and managing these bleeding varices are complicated and may require advanced techniques, such as double balloon enteroscopy (DBE), where banding is not compatible with the endoscopes. Often co-management with radiology for coil embolization or surgical resection may be required.
We report a case of successful control of a jejunal variceal bleed by identifying the varix on CT angiography (CTA), treating it endoscopically with sclerosing agent with subsequent placement of a fiducial clip, followed by definitive treatment with coil embolization.
Case Description/Methods: A 59-year-old male with alcoholic cirrhosis and a non-incarcerated ventral hernia from prior abdominal surgeries was transferred for large volume hematochezia requiring massive transfusion protocol and pressor support in the medical intensive care unit. Esophagogastroduodenoscopy (EGD) showed fresh red blood with large clots in the proximal jejunum with no active bleed. A CTA of the abdomen and pelvis was performed, which identified an actively bleeding jejunal varix within the ventral hernia (Image 1).
A DBE located a large jejunal varix within the ventral hernia. This was treated with a sclerosing agent and placing a hemostatic clip as a fiducial. Although successful, we consulted radiology for embolization due to the high-risk features of the varix (Image 2). Ten coils were deployed within the distal branches of the superior mesenteric vein (SMV). Initial access to the inferior mesenteric vein created iatrogenic venous injury leading to bleeding in the small bowel, requiring the left inferior epigastric vein to access to the peripherals of the superior mesenteric vein. Surgery was consulted, but determined the patient was not a surgical candidate.
Discussion: While ectopic varices account for 1-5% of all variceal bleeds, those arising from the jejunum are remarkably rare. This case demonstrates jejunal variceal bleeding can be treated by endoscopic evaluation and embolization, even in cases of abnormal abdominal and vascular anatomy.
When surgery is not an option, DBE can allow for visualization of jejunal varices. Due to lack of treatment options via DBE, placing a fiducial clip may assist radiology in identifying and coiling the problematic varices.

Figure: A. Axial Image of CT Angiography demonstrating the varix within the left upper quadrant within a large abdominal hernia.
B. Endsocopic image obtained during double balloon enteroscopy revealing the jejunal varix with high risk stigmata of bleeding as well as fresh blood within the lumen.
B. Endsocopic image obtained during double balloon enteroscopy revealing the jejunal varix with high risk stigmata of bleeding as well as fresh blood within the lumen.
Disclosures:
Scott Weismiller indicated no relevant financial relationships.
Ibrahim Yaghnam indicated no relevant financial relationships.
Ian Schreibman indicated no relevant financial relationships.
Scott Weismiller, MD1, Ibrahim Yaghnam, MD2, Ian Schreibman, MD1. P2099 - Seeing the Unseen: Management of a Jejunal Variceal Bleed with Endoscopic Sclerosing Therapy Followed by Coil Embolization, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

